Objective 2: Improve Care for Hard-to-Manage Symptoms

Managing symptoms—particularly recurring or chronic symptoms such as back, neck, or joint pain, anxiety, headache, and insomnia—is challenging. Symptoms may change over time, and patients may experience multiple symptoms in clusters (e.g., pain, sleep difficulties, and mood changes) rather than a single symptom in isolation. Current approaches to symptom management often have limitations. Despite medical treatment, some patients continue to experience troublesome levels of symptoms and a diminished quality of life. Moreover, medications used to treat symptoms may have significant risks and side effects.
Expanding the knowledge base about how complementary health approaches may improve symptom management in both the short and long term is a priority for NCCIH. There is a growing body of basic and clinical research on complementary health approaches for symptom management that employs the methods, tools, and technology of neuroscience, psychoneuroimmunology, psychology, behavioral medicine, physical medicine, and biomechanics. For example, research studies have revealed that interventions such as meditation and acupuncture affect central mechanisms of pain perception and processing, regulation of emotion and attention, and placebo responses. Although not yet fully understood, these effects point toward scientifically plausible mechanisms—often unrelated to traditional explanations or hypotheses concerning their mechanisms of action—by which these interventions might be effective.
STRATEGIES
1. Develop and improve complementary health approaches and integrative treatment strategies for managing symptoms such as pain, anxiety, and depression.
NCCIH is particularly interested in clinical studies of interventions for pain, anxiety, and depression, as treatment options for these conditions are limited and some have deleterious side effects. NCCIH is also interested in better understanding the transition from acute to chronic pain and testing and developing interventions that may prevent it.
Rigorous study of any clinical intervention requires the use of well-established methodology. Well-powered randomized clinical studies are recognized as an essential component of the evidence base regarding clinical efficacy or effectiveness. To implement such studies, the magnitude and nature of treatment effects must be estimated in preliminary studies, treatment algorithms must be developed and validated, and feasibility of volunteer recruitment must be established. Methods are needed to measure consistency and fidelity of protocol implementation, practitioner variability, and adherence of participants to the interventions being studied. In addition, well-characterized and meaningful clinical and laboratory outcome measures are needed to fully determine safety and to definitively measure benefit or the lack thereof.
Mind and Body Practices
Emerging evidence of promising clinical effects of many mind and body approaches points toward important opportunities to advance the science and improve the practice of symptom management. In many cases the evidence is strengthened by results from basic and clinical research that employ the tools and technology of neuroscience, immunology, psychology, behavioral and physical medicine, and biomechanics. Addressing the scientific and operational challenges confronting the study of promising mind and body interventions requires continued efforts to foster multidisciplinary collaborations that engage the expertise and experience of complementary health practitioners and use the tools and technologies of a variety of scientific disciplines.
Natural Products, Including Probiotics
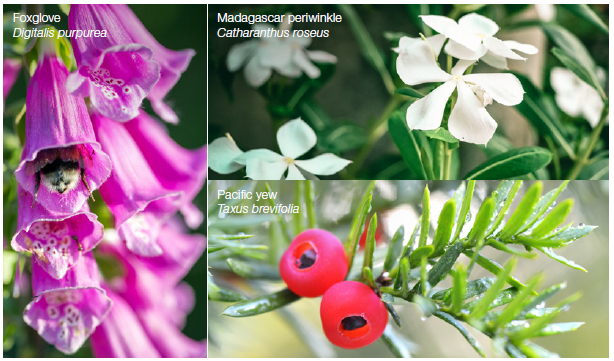
NCCIH seeks to support clinical studies of the use of natural products for symptom management. The aim of such research is to confirm the link between the impact of the natural product on a biological signature (i.e., mechanism of action) and demonstrate an association between the change in the biological signature and clinical outcomes in humans. Large clinical trials are warranted only when basic and translational research enables rigorous testing of evidence-based hypotheses.
2. Conduct studies in “real world” clinical settings to test the safety and efficacy of complementary health approaches, including their integration into health care.
The Center is particularly interested in studies on the efficacy and effectiveness of complementary and integrative health approaches aimed at managing pain, anxiety, and depression. There are many practical questions emerging from the NCCIH pain portfolio that could be studied using a pragmatic approach. For example, there is growing evidence, reflected in systematic reviews, that a number of mind and body therapies are beneficial for pain management, including acupuncture and meditation for the management of chronic low-back pain.
Many research organizations, including NIH, support the concept of a learning health care system in which research is embedded into the delivery of care. In this type of system, data are collected every time a patient receives care, and over time, the system “learns” whether and how well the care worked. Whenever something is learned with this approach, it can be quickly applied and adopted.
Integrating an effectiveness study within a health care system is often challenging. Research and patient care have long been conceptualized as separate activities that take place in different locations under different types of oversight, and the types of recordkeeping used in clinical care, including electronic health records, may not always meet research needs. However, these challenges are beginning to be overcome, and innovative approaches are being developed allowing for informative research to be conducted in the actual settings where integrative health care is practiced. These approaches include pragmatic trials that employ rigorous experimental designs.
Given the widespread use of complementary health approaches, opportunities exist to employ clinical outcomes and effectiveness research methodologies to collect “real world” evidence about the use of specific complementary approaches for health care and health promotion. Pursuing this type of research requires creative collaboration with those who provide care in settings where integration of complementary health approaches could be studied. The “real world” settings for such research may be quite varied, and could include schools, nursing homes, hospices, safety net clinics, cancer treatment facilities, and settings that provide care for military personnel and Veterans. NCCIH seeks to build upon the success of initiatives taking on this challenge such as the NIH Health Care Systems Research Collaboratory, an NIH Common Fund initiative that is co-led by NCCIH.