Congressional Justification FY 2022
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health (NCCIH)
On this page:
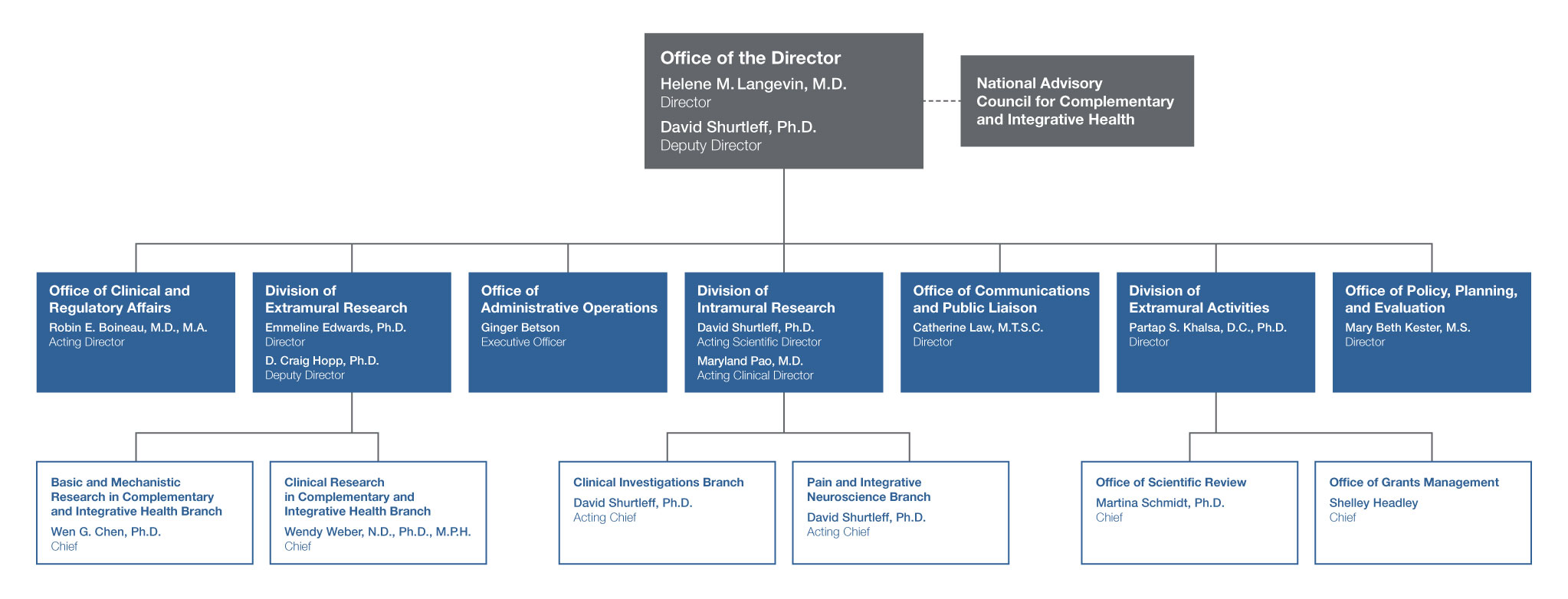
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Mechanism Table
- Major Changes in Budget Request
- Summary of Changes
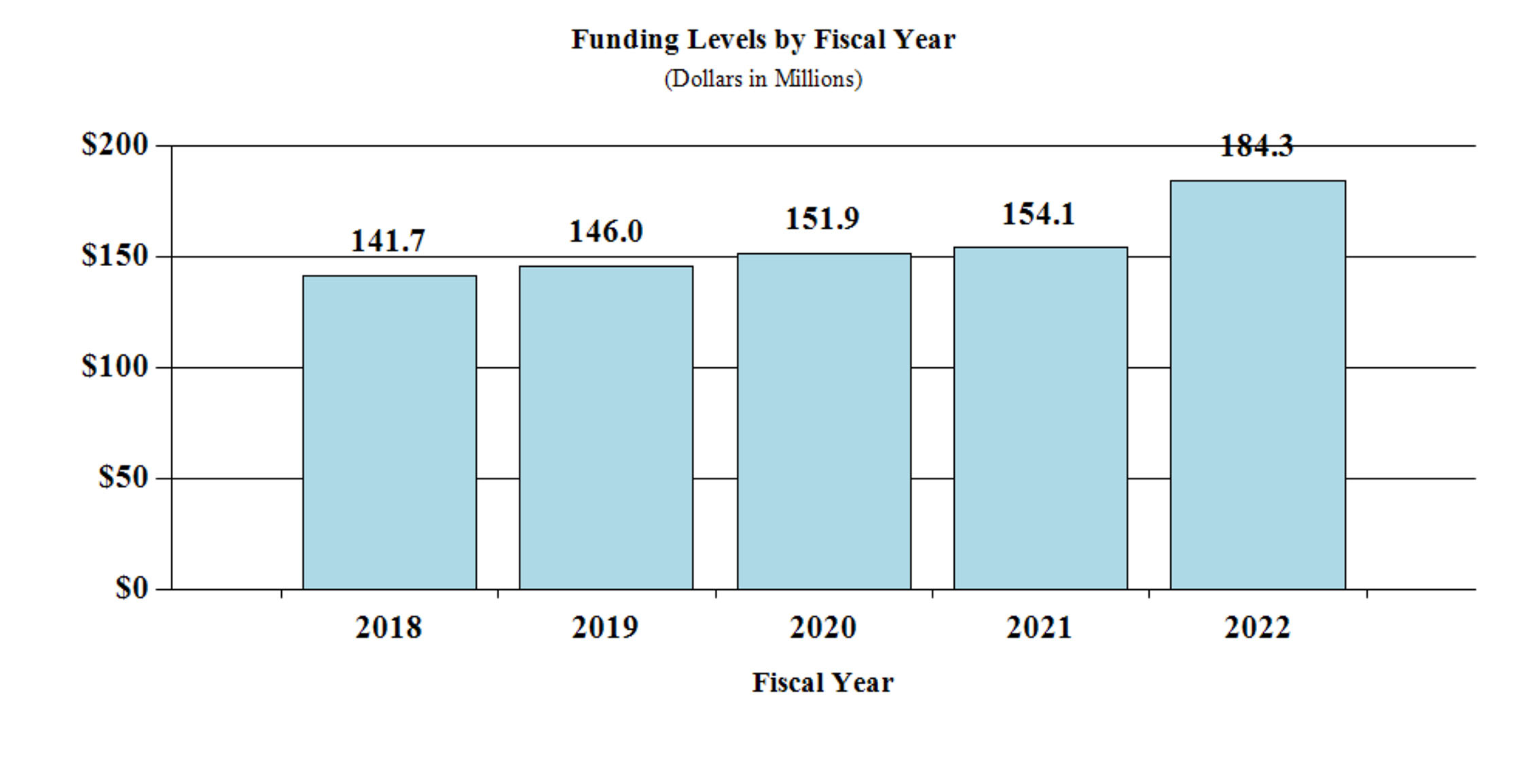
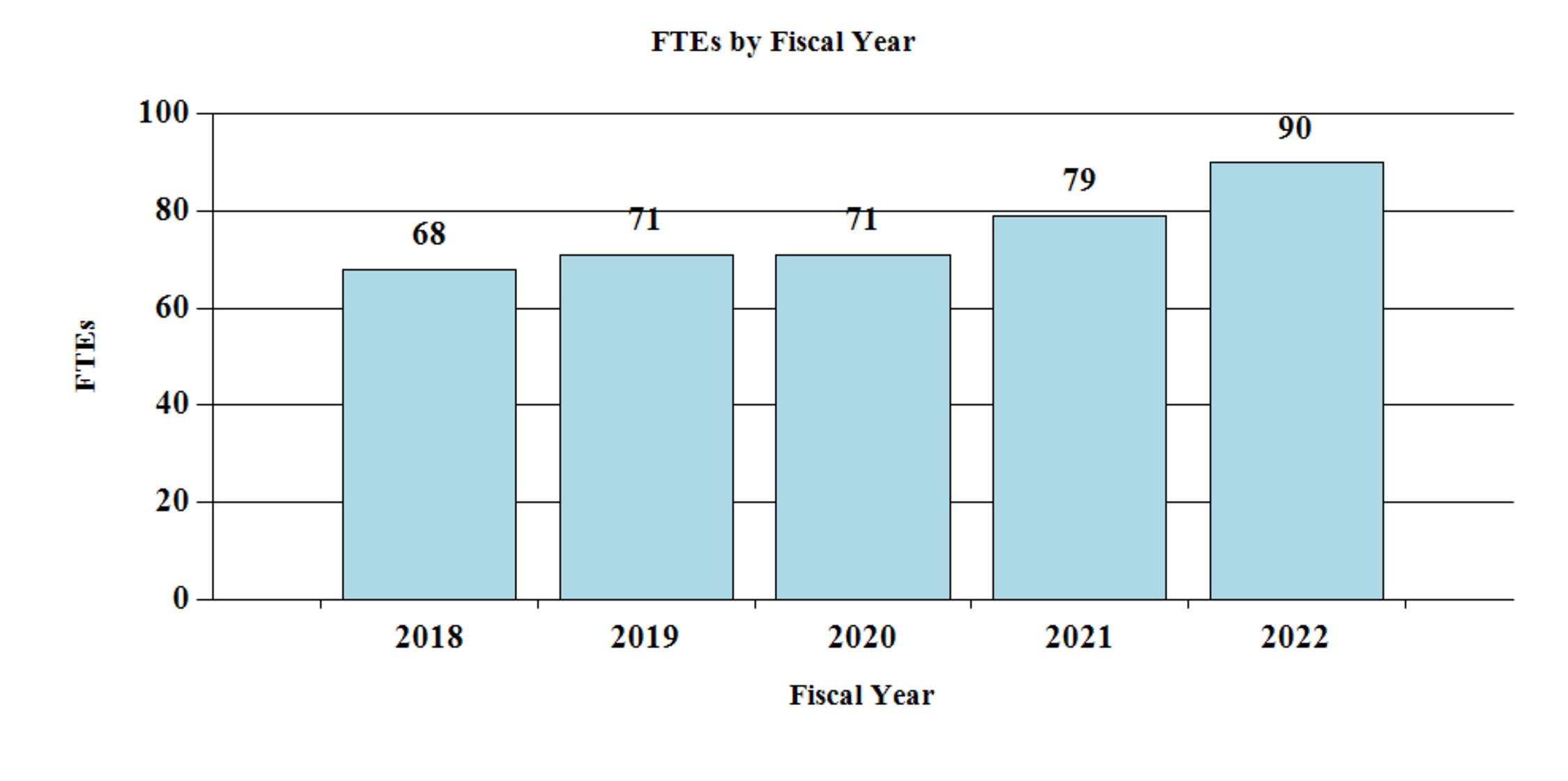
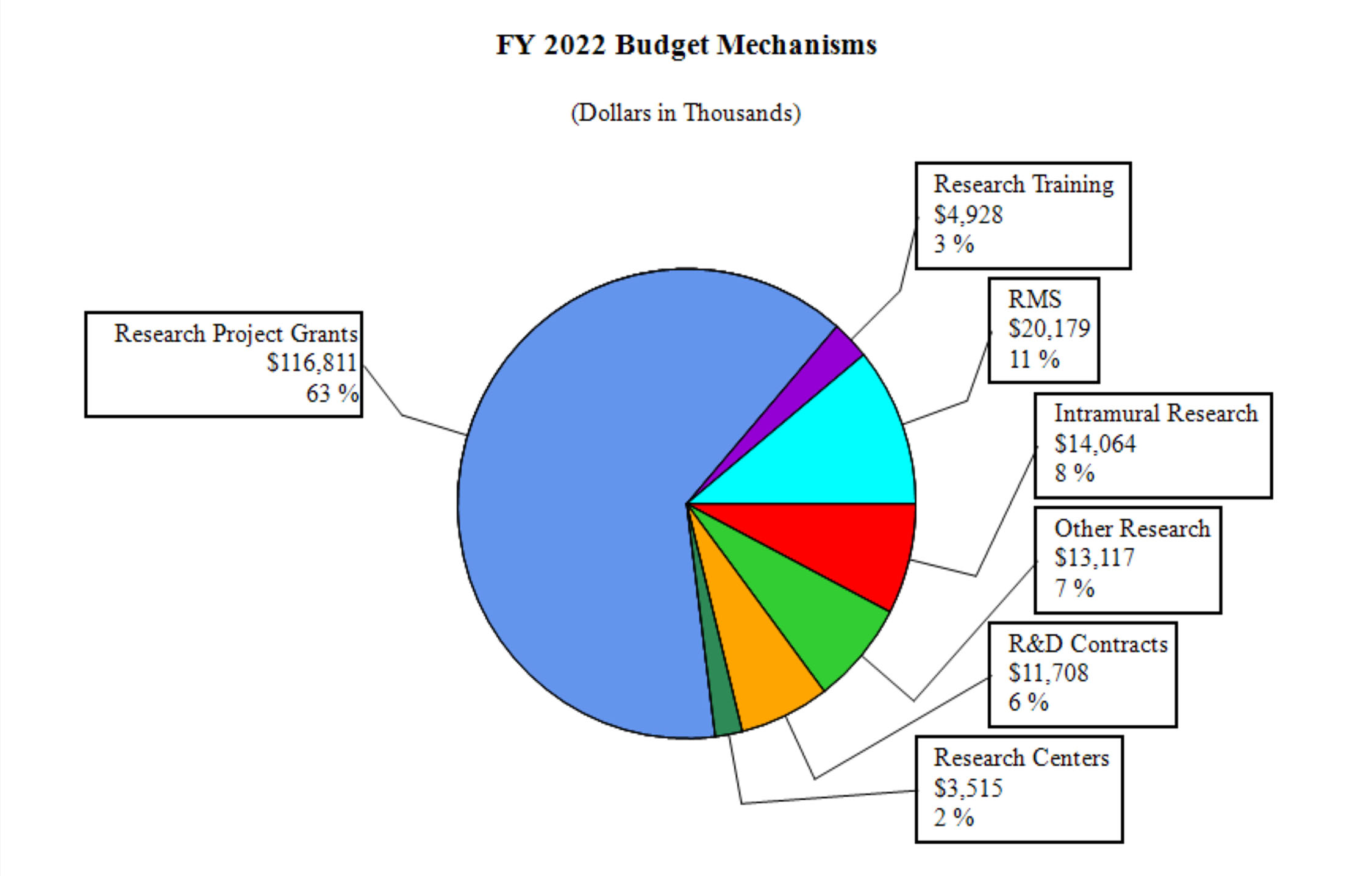
- Budget Graphs
- Budget Authority by Activity
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
NATIONAL INSTITUTES OF HEALTH
NATIONAL CENTER FOR COMPLEMENTARY AND INTEGRATIVE HEALTH
For carrying out section 301 and title IV of the PHS Act with respect to complementary and integrative health, [$154,162,000] $184,323,000.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Amounts Available for Obligation 1
(Dollars in Thousands)
| Source of Funding | FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget |
|---|---|---|---|
| Appropriation | $151,740 | $154,162 | $184,323 |
| OAR HIV/AIDS Transfers | 137 | -83 | 0 |
| Subtotal, adjusted budget authority | $151,877 | $154,079 | $185,323 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $151,877 | $154,079 | $184,323 |
| Unobligated balance lapsing | -6 | 0 | 0 |
| Total obligations | $151,871 | $154,079 | $184,323 |
| 1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2020 — $1,330 FY 2021 — $1,320 FY 2022 — $995 | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Mechanism - Total 1
(Dollars in Thousands)
| MECHANISM | FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY 2021 Enacted | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 138 | $66,761 | 136 | $65,655 | 129 | $62,555 | -7 | $3,100 |
| Administrative Supplements | (22) | 4,110 | (21) | 3,865 | (11) | 2,000 | (-10) | -1,865 |
| Competing: | ||||||||
| Renewal | 1 | 419 | 0 | 0 | 0 | 0 | 0 | 0 |
| New | 38 | 17,319 | 41 | 18,611 | 103 | 46,813 | 62 | 28,202 |
| Supplements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Subtotal, Competing | 39 | $17,738 | 41 | $18,611 | 103 | $46,813 | 62 | $28,202 |
| Subtotal, RPGs | 177 | $88,610 | 177 | $88,130 | 232 | $111,368 | 55 | $23,238 |
| SBIR/STTR | 9 | 4,328 | 9 | 4,381 | 11 | 5,443 | 2 | 1,062 |
| Research Project Grants | 186 | $92,938 | 186 | $92,512 | 243 | $116,811 | 57 | $24,299 |
| Research Centers: | ||||||||
| Specialized/Comprehensive | 1 | $1,372 | 3 | $3,328 | 3 | $3,515 | 0 | $187 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 1 | 995 | 0 | 0 | 0 | 0 | 0 | 0 |
| Comparative Medicine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers in Minority Institutions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers | 2 | $2,366 | 3 | $3,328 | 3 | $3,515 | 0 | $187 |
| Other Research: | ||||||||
| Research Careers | 38 | $6,311 | 34 | $5,671 | 35 | $5,830 | 1 | $159 |
| Cancer Education | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cooperative Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Minority Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 7 | 3,311 | 11 | 5,199 | 15 | 7,287 | 4 | 2,088 |
| Other Research | 45 | $9,622 | 45 | $10,870 | 50 | $13,117 | 5 | $2,247 |
| Total Research Grants | 233 | $104,926 | 234 | $106,710 | 296 | $133,443 | 62 | $26,733 |
| Ruth L Kirchstein Training Awards: | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 27 | $1,220 | 22 | $974 | 23 | $1,021 | 1 | $47 |
| Institutional Awards | 46 | 3,580 | 48 | 3,726 | 49 | 3,907 | 1 | 181 |
| Total Research Training | 73 | $4,800 | 70 | $4,700 | 72 | $4,928 | 2 | $228 |
| Research & Develop. Contracts | 10 | $10,754 | 10 | $10,644 | 11 | $11,708 | 1 | $1,064 |
| (SBIR/STTR) (non-add) | (0) | (45) | (0) | (45) | (0) | (56) | (0) | (11) |
| Intramural Research | 8 | 12,792 | 11 | 12,785 | 14 | 14,064 | 3 | 1,279 |
| Res. Management & Support | 63 | 18,605 | 68 | 19,240 | 76 | 20,179 | 8 | 940 |
| SBIR Admin (non-add) | (0) | (56) | (0) | (56) | (0) | (70) | (0) | (14) |
| Construction | 0 | 0 | 0 | 0 | ||||
| Buildings and Facilities | 0 | 0 | 0 | 0 | ||||
| Total, NCCIH | 71 | $151,877 | 79 | $154,079 | 90 | $184,323 | 11 | $30,244 |
1 All items in italics and brackets are non-add entries.
Major Changes in the Fiscal Year 2022 President’s Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanisms and activity detail and these highlights will not sum to the total change for the FY 2022 budget request for NCCIH, which is $184.3 million, an increase of $30.2 million from the FY 2021 Enacted level. Within the request level, NCCIH will pursue its highest research priorities through strategic investments and careful stewardship of appropriated funds.
Research Project Grants (+$24.3 million; total $116.8 million): NCCIH will support a total of 243 Research Project Grant (RPG) awards in FY 2022. Noncompeting RPGs will decrease by $3.1 million, while Competing RPG awards will increase by $28.2 million.
R&D Contracts (+$1.1 million; total $11.7 million): NCCIH will continue its annual support to the National Health Interview Survey (NHIS) and other mission-supporting Research and Development Contracts.
Intramural Research (+$1.3 million; total $14.1 million): NCCIH will continue to support intramural research activities, including Dr. Langevin’s Research Lab.
Research Management and Support (+$0.940 million; total $20.1 million): NCCIH will manage a full-time equivalent staff level of 76 and fund inflation-related costs.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Summary of Changes
(Dollars in Thousands)
| FY 2021 Enacted | $154,079 | ||||||
|---|---|---|---|---|---|---|---|
| FY 2022 President’s Budget | $184,323 | ||||||
| Net Change | $30,244 | ||||||
| CHANGES | FY 2021 Enacted | FY 2022 President’s Budget | Built-In Change from FY 2021 Enacted | ||||
| FTEs | Budget Authority | FTEs | Budget Authority | FTEs | Budget Authority | ||
| A. Built-in: | |||||||
| 1. Intramural Research: | � | ||||||
| a. Annualization of January 2021 pay increase & benefits | $3,530 | $4,303 | $10 | ||||
| b. January FY 2022 pay increase & benefits | 3,530 | 4,303 | 90 | ||||
| c. Paid days adjustment | 3,530 | 4,303 | 0 | ||||
| d. Differences attributable to change in FTE | 3,530 | 4,303 | 963 | ||||
| e. Payment for centrally furnished services | 2,264 | 2,377 | 113 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 6,992 | 7,384 | 293 | ||||
| Subtotal | $1,469 | ||||||
| 2. Research Management and Support: | |||||||
| a. Annualization of January 2021 pay increase & benefits | $12,123 | $12,637 | $33 | ||||
| b. January FY 2022 pay increase & benefits | 12,123 | 12,637 | 348 | ||||
| c. Paid days adjustment | 12,123 | 12,637 | 0 | ||||
| d. Differences attributable to change in FTE | 12,123 | 12,637 | 1,267 | ||||
| e. Payment for centrally furnished services | 607 | 637 | 30 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 6,510 | 6,905 | 238 | ||||
| Subtotal | $1,915 | ||||||
| Subtotal, Built-in | $3,384 | ||||||
| CHANGES | FY 2021 Enacted | FY 2022 President’s Budget | Program Change from FY 2021 Enacted | |||
|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 136 | $69,519 | 129 | $64,555 | -7 | -$4,965 |
| b. Competing | 41 | 18,611 | 103 | 46,813 | 62 | 28,202 |
| c. SBIR/STTR | 9 | 4,381 | 11 | 5,443 | 2 | 1,062 |
| Subtotal, RPGs | 186 | $92,512 | 243 | $116,811 | 57 | $24,299 |
| 2. Research Centers | 3 | $3,328 | 3 | $3,515 | 0 | $187 |
| 3. Other Research | 45 | 10,870 | 50 | 13,117 | 5 | 2,247 |
| 4. Research Training | 70 | 4,700 | 72 | 4,928 | 2 | 228 |
| 5. Research and development contracts | 10 | 10,644 | 11 | 11,708 | 1 | 1,064 |
| Subtotal, Extramural | $122,054 | $150,080 | $28,026 | |||
| FTEs | FTEs | FTEs | ||||
| 6. Intramural Research | 11 | $12,785 | 14 | $14,064 | 3 | -$190 |
| 7. Research Management and Support | 68 | 19,240 | 76 | 20,179 | 8 | -976 |
| 8. Construction | 0 | 0 | 0 | |||
| 9. Buildings and Facilities | 0 | 0 | 0 | |||
| Subtotal, Program | 79 | $154,079 | 90 | $184,323 | 11 | $26,860 |
| Total built-in and program changes | $30,244 | |||||
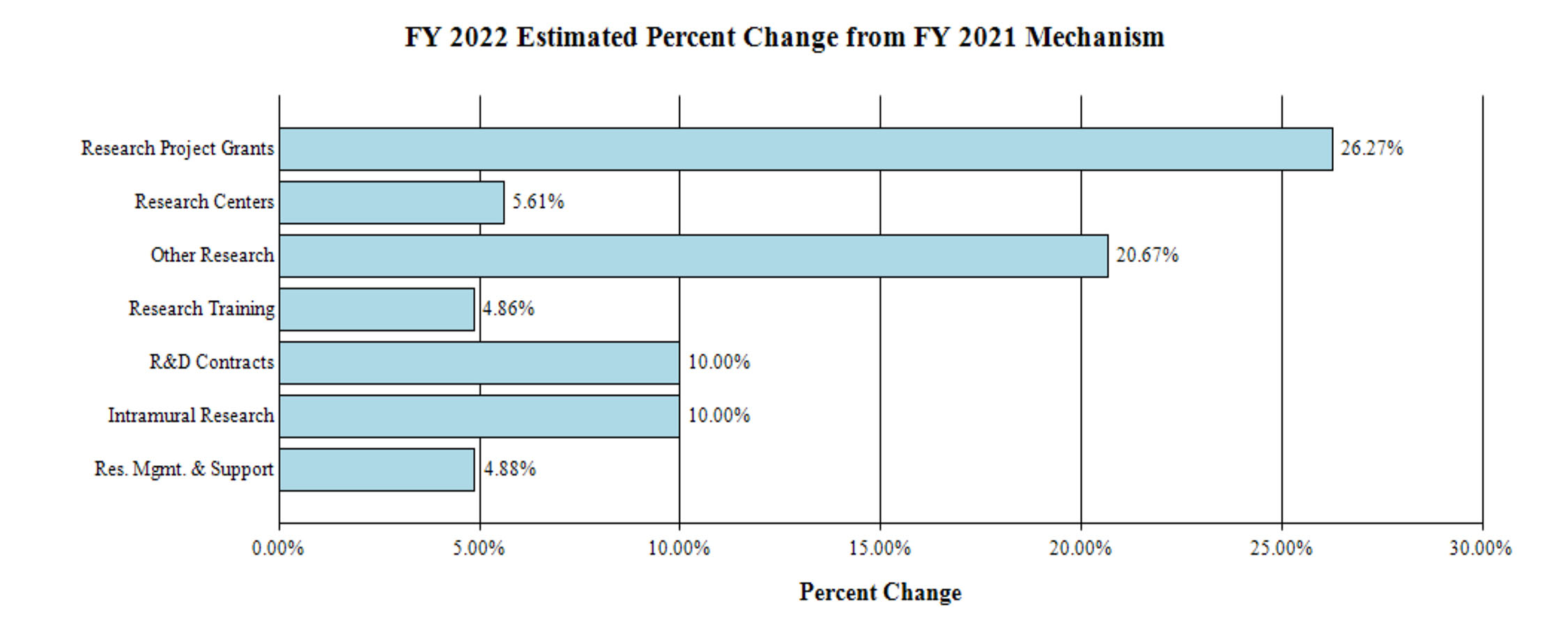
Fiscal Year 2022 Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanisms:
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Activity1
(Dollars in Thousands)
| FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY2021 | |||||
|---|---|---|---|---|---|---|---|---|
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | ||||||||
| Detail | ||||||||
| Clinical Research | $65,517 | $65,995 | $79,879 | $13,884 | ||||
| Basic Research | 50,163 | 51,359 | 65,273 | 13,913 | ||||
| Extramural Research Training and Capacity Building | 4,800 | 4,700 | 4,928 | 228 | ||||
| Subtotal, Extramural | $120,480 | $122,054 | $150,080 | $28,026 | ||||
| Intramural Research | 8 | $12,792 | 11 | $12,785 | 14 | $14,064 | 3 | $1,279 |
| Research Management & Support | 63 | $18,605 | 68 | $19,240 | 76 | $20,179 | 8 | $940 |
| TOTAL | 71 | $151,877 | 79 | $154,079 | 90 | $184,323 | 11 | $30,244 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2021 Amount Authorized | FY 2021 Enacted | 2022 Amount Authorized | FY 2022 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | Indefinite | ||||
| $154,079,000 | $184,323,000 | |||||||
| National Center for Complementary and Integrative Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total, Budget Authority | $154,079,000 | $184,323,000 | ||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation | ||||
|---|---|---|---|---|---|---|---|---|
1 Budget Estimate to Congress includes mandatory financing. | ||||||||
| 2013 | $127,930,000 | $128,318,000 | $128,056,515 | |||||
| Rescission | $256,113 | |||||||
| Sequestration | ($6,427,556) | |||||||
| 2014 | $129,041,000 | $128,183,000 | $124,296,000 | |||||
| Rescission | $0 | |||||||
| 2015 | $124,509,000 | $124,681,000 | ||||||
| Rescission | $0 | |||||||
| 2016 | $127,521,000 | $127,585,000 | $130,162,000 | $130,789,000 | ||||
| Rescission | $0 | |||||||
| 20171 | $129,941,000 | $134,549,000 | $136,195,000 | $134,689,000 | ||||
| Rescission | $0 | |||||||
| 2018 | $101,793,000 | $136,741,000 | $139,654,000 | $142,184,000 | ||||
| Rescission | $0 | |||||||
| 2019 | $130,717,000 | $143,882,000 | $146,550,000 | $146,473,000 | ||||
| Rescission | $0 | |||||||
| 2020 | $126,081,000 | $153,632,000 | $154,695,000 | $151,740,000 | ||||
| Rescission | $0 | |||||||
| 2021 | $138,167,000 | $153,045,000 | $156,823,000 | $154,162,000 | ||||
| Rescission | $0 | |||||||
| 2022 | $184,323,000 | |||||||
Justification of Budget Request
National Center for Complementary and Integrative Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY 2021 | |
|---|---|---|---|---|
| BA | $151,877,000 | $154,079,000 | $184,323,000 | +$30,244,000 |
| FTE | 71 | 79 | 90 | +11 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Director's Overview
The mission of the National Center for Complementary and Integrative Health (NCCIH) is to define, through rigorous scientific investigation, the fundamental mechanisms, safety, and effectiveness of complementary and integrative health approaches.
Americans spend approximately $30.2 billion per year on complementary health approaches.1 This diverse group of health practices includes dietary, psychological, and physical treatments and practices that may have originated outside of conventional medicine, such as dietary supplements, plant-based products, probiotics, yoga, massage therapy, meditation, mindfulness-based stress reduction, spinal manipulation, and acupuncture. These approaches are typically used in conjunction with conventional medicine to promote health and well-being, manage symptoms of a disease or condition, and alleviate side effects of medications. Integrative health care seeks to bring conventional and complementary approaches together in a safe, coordinated way with the goal of improving clinical care for patients, promoting health, and preventing disease.
As a responsible steward of resources, we are highly selective and support a broad range of scientifically meritorious basic, clinical, and translational research. We focus on areas with the greatest impact by prioritizing research topics that show scientific promise and are amenable to rigorous scientific inquiry. We strive to invest in research that will drive new discoveries and may lead to improved public health and health care.
Responding to Pressing Health Needs
Non-Opioid Pain Management
Chronic pain is a major public health problem in the United States. An estimated 126 million U.S. adults suffer from a painful condition and over 25 million Americans suffer from daily chronic pain.2 Together, pain costs the United States more than $600 billion per year in treatments and lost productivity.3 In addition, the use of highly addictive opioids as a primary pain management strategy for severe or chronic pain is fueling the growing opioid misuse epidemic. There is an urgent need for new and improved pain management strategies.
NCCIH is leading multiple pragmatic pain management clinical research efforts. Pragmatic clinical trials are human effectiveness trials that can be embedded in standard health care. These studies are beneficial because they are conducted in a real-world setting with a real-world distribution of patients. NCCIH leads the NIH-Department of Defense-Veterans Affairs Pain Management Collaboratory (PMC) partnership to support research evaluating the efficacy of non-drug pain management within the military and veteran health care systems and to investigate how these approaches could be integrated into the health care systems. We are also leading the NIH Helping to End Addiction Long-termSM (HEAL) Initiative’s Pragmatic and Implementation Studies for the Management of Pain to Reduce Opioid Prescribing (PRISM) program that seeks to take interventions and treatment guidelines that have already been shown to work for specific pain conditions and integrate them into health care delivery systems.
NCCIH also supports research on behavioral strategies to manage chronic pain, improve adherence to the medical treatment of opioid use disorders, and reduce the psychological and physical cravings for opioids. These strategies are especially important for patients who have successfully quit using opioids, but who continue to have pain and need options for pain management that will not increase their likelihood of relapse. NCCIH is also leading the NIH HEAL Initiative’sSM Behavioral Research to Improve Medication-Based Treatment (BRIM) program. This program seeks to understand whether adding behavioral interventions such as cognitive behavioral therapy or meditation can help improve outcomes for patients with opioid use disorder (OUD) by helping them stay on their medications for treating OUD.
In addition to these efforts, NCCIH has expanded research efforts around natural products for pain management. We launched two new funding initiatives to support this research; one focused on the potential pain-relieving properties of natural products in general, and the other focused on evaluating terpenes and minor cannabinoids for their potential non-psychogenic effects, such as analgesia.
COVID-19 Crisis
In 2020, the novel SARS-CoV-2 virus started a global pandemic, which is still ongoing. The pandemic has presented a health crisis as more than 160 million people around the world have become ill and millions have died. The social distancing measures put in place to try to stop the spread of the virus also affected daily life, shutting down businesses, schools, and cities. NIH mobilized resources to develop vaccines, therapeutics, and other treatment strategies to manage the pandemic. In addition, NIH supported research to address and study the biological, behavioral, psychosocial, and socioeconomic impacts of the pandemic. NCCIH participated in these efforts through funding opportunities that focused on natural products for the treatment or management of COVID-19, supporting research on behavioral interventions focused on stress management and emotional resilience, promoting research on studying and implementing digital health care interventions, and addressing health disparities with regard to access to COVID-19 testing, and treatment among minority populations.
Working To Address Health Disparities
NCCIH is committed to funding research with diverse populations and promoting a diverse scientific workforce. We support training, career development, and research opportunities directed at minority health, and health disparities.
Training and career development for underrepresented minorities
NCCIH supports research training and career development programs to increase the number and diversity of well-trained scientists to conduct rigorous complementary and integrative health research. We have special opportunities for individuals from groups who are underrepresented in scientific research (e.g., racial and ethnic minority populations) throughout the continuum from high school to faculty. In addition, we support workshops at NIH and at scientific conferences to help students and fellows connect to NIH funding opportunities, understand how to interact with NIH staff to develop research proposals, navigate the NIH peer-review process successfully, develop resilience to overcome career roadblocks, and develop plans for a successful research career. We attend a wide variety of scientific conferences and have targeted outreach to minority-oriented societies such as the Society for Advancement of Chicanos/Hispanics and Native Americans in Science (SACNAS) and the Annual Biomedical Research Conference for Minority Students (ABRCMS).
Research involving minority health and health disparities
NCCIH seeks to expand the research we support involving understudied, underrepresented, and underreported populations. We participate in initiatives targeted toward these populations and are currently supporting research to explore the development, feasibility, optimization, and efficacy of complementary and integrative health interventions within minority-, low socioeconomic-, rural-, urban-, and gender-specific populations. In addition, we encourage research in these populations through outreach activities. For example, NCCIH co-sponsored the “NIH 2019 Traditional Medicine Summit” with the NIH Tribal Health Research Office. The goals of this summit were to identify approaches to respectful collaboration between traditional medicine practitioners and health researchers; explore the relationships between traditional medicine and health care services; and connect younger generations of American Indian/Alaska Native people to traditional medicine, integrative health research, and academic research. We plan to continue expanding these efforts.
Capitalizing on Basic and Foundational Research and Investing in the Future
NCCIH’s investment in basic research has supported the development of new complementary and integrative health approaches and the optimization of others. Basic research has expanded our knowledge of natural products, including potentially dangerous herb-drug interactions. Research on the mechanisms of meditation has advanced our scientific knowledge of brain circuits related to emotion, the reward response, and pain. Years of investment in understanding the basic biology of pain and pain management techniques have led to the advancement of promising approaches through pragmatic clinical trials and implementation science. Acupuncture, for example, has been shown to help ease low-back pain, neck pain, migraine, and osteoarthritis/knee pain in specific populations. As a result, the Centers for Medicare & Medicaid Services began covering acupuncture for the management of chronic low-back pain in older adults in 2019. Altogether, investments made in basic research have expanded the scientific evidence of complementary health approaches leading to increased use and acceptance as evidenced by a recent NCCIH-sponsored study that showed that more than half of office-based physicians recommend at least one complementary health approach to their patients.4
As we look to the future, we see new areas for investment. The COVID-19 crisis has highlighted a need for independent care options, such as mobile health applications, self-care approaches, and telehealth. NCCIH is investing in the development, optimization, and utilization of these approaches for evidence-based complementary and integrative health approaches. NCCIH is also looking to expand research efforts around health with a particular interest in music and the arts, as well as research on whole person health.
Music has the remarkable ability to enhance child development, improve adult function and well-being, and optimize the quality of life during aging. Studies have shown that music can also ameliorate the symptoms of a broad range of diseases and disorders that occur throughout the lifespan. To explore this exciting avenue of research, NCCIH and our NIH partners have developed the Sound Health initiative. This funding opportunity supports research to understand how music impacts our mind and body, its role in health and development, and its potential to treat disease symptoms.
NCCIH plans to support whole person health research, which we see as a complement to individualized and precision medicine. Whole person health research focuses on health as a biopsychosocial process that involves the whole person. By deepening our scientific understanding of the connections that exist across domains of human health, we can better understand how conditions interrelate, define multimodal interventions that address these problems, and improve how we support patients through the full continuum of their health experience, including the return to health.
Overall Budget Policy: The FY 2022 President’s Budget request for NCCIH is $184.3 million, an increase of $30.2 million or 19.6 percent above the FY 2021 Enacted level. $26.0 million of this increase will be allocated to expanding NCCIH research into pain and pain management.
Program Descriptions and Accomplishments
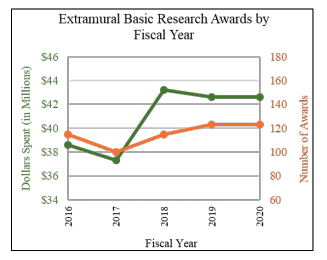
Extramural Basic Research: Basic research on the fundamental biological effects of active components of interventions is central to the development of the evidence base on complementary and integrative health approaches and underpins the design of clinical research. While NCCIH continues its broad support of investigator-initiated research, the Center will also support translational research to optimize therapeutic effects through targeted initiatives. For example, NCCIH supports translational research to ascertain the biological effects of nonpharmacologic therapies on the brain with the ultimate goal of optimizing their effects. NCCIH is also energizing the research community to overcome the methodologic and technologic obstacles hindering basic research on natural products and nonpharmacologic therapies, as well as encouraging the incorporation of cutting-edge technologies to monitor and enhance these interventions. The following are recently published results from NCCIH-supported basic extramural research.
Researchers at the University of Pittsburgh Brain Institute investigated the nervous system connections between rats’ brains and stomachs. Most research on the gut–brain connection has focused on how the gut influences brain function. This study sought to identify how the brain influences gut function. Using a viral tagging system that travels from one neuron to another from the rats’ stomachs to their brains, the scientists identified the brain areas that most directly influence involuntary control of the rat stomach. They found that this control was influenced primarily by two areas of the brain that are involved in regulating emotion and interoception (the perception of sensations from inside the body). These data highlight an interesting loop in which the brain’s control of the stomach and its environment can be influenced by mental and emotional processes. The researchers noted that the findings from this study may provide targets for brain-based therapies for gastrointestinal disorders, which could involve altering stomach function and/or the microbiome using noninvasive transcranial stimulation alone or combined with cognitive-, behavioral-, and movement-based therapies.5
Scientists from Rutgers University examined the impact of abnormal Paneth cell lysozyme production on gut bacteria and intestinal inflammation. Paneth cells mostly reside in the small intestine and produce different antimicrobial proteins, including lysozyme. They play a critical role in the defense against a broad range of gut microbes. Paneth cell metaplasia (the presence of Paneth cells in the large intestine where they are not normally found in healthy individuals) is a characteristic feature of inflammatory bowel diseases, including ulcerative colitis and Crohn’s disease. In this study, researchers found that disruption of Paneth cell lysozyme protected mice from colitis. The researchers further investigated the protective mechanism involved in gut commensal bacteria. They found that the aberrant lysozyme secretion by Paneth cells in the colon suppresses the growth of certain bacterial species, resulting in imbalance in the gut microbiota which leads to mucosal inflammation during colitis. The insights gained from this study may be helpful in developing new therapies for inflammatory bowel diseases, which affect 1.6 million people in the United States. However, further research is needed to determine whether the effects of Paneth cell lysozyme in humans are the same as those seen in the mouse models.6
Findings from a study conducted in rats suggest that dietary supplementation with polyphenols (naturally occurring compounds found in plant-derived foods) may reduce back pain associated with intervertebral disc (IVD) degeneration. IVD is a common condition characterized by the breakdown of one or more of the discs that separate the bones of the spine, causing pain in the back or neck and often in the legs and arms. The study was a multisite collaboration involving researchers from the Icahn School of Medicine at Mount Sinai, Philadelphia College of Osteopathic Medicine, Veterans Affairs Medical Center (The Bronx), University of Pennsylvania, and Keiyu Orthopedic Hospital in Tatebayashi, Japan. While it is not yet fully understood how polyphenols work in the body, the researchers noted that the promising effect of reducing back pain from IVD injury warrants further study.7
Scientists at Harvard Medical School and Baylor College of Medicine investigated how acupuncture stimulation at specific body regions drives distinct nervous system pathways, with a particular focus on prevention and treatment of systemic inflammation. The researchers used systemic inflammation in mice as a model and found that acupuncture stimulation either reduces or increases systemic inflammation, depending on the dose, through specific nervous system pathways. The researchers also suggested that electroacupuncture has an advantage over manual acupuncture in that the intensity of electroacupuncture is easier to control. These findings may help to improve acupuncture practice and inform efficacy and safety trials for acupuncture as a therapeutic treatment.8
Evaluating the Therapeutic Potential of Cannabis

There is growing interest in the potential medical utility of cannabis and its constituents. The public perception that cannabis has a therapeutic benefit has led to its legalization in 33 U.S. states and the District of Columbia for medical reasons. However, there is little evidence to support the safety or efficacy of cannabis for the management of many of the symptoms and disorders for which it is used.
Pain is an exception. A growing body of literature suggests that the cannabis plant may have pain-relieving properties; however, cannabis is a Schedule I substance with known abuse potential and negative psychoactive effects. The question remains if the potential pain-relieving properties of cannabis can be separated from its negative properties. To address this question, more research is needed into the basic biological activity of the plant’s diverse phytochemicals.
The cannabis plant contains more than 100 each of cannabinoids and terpenes (substances in cannabis that give the plant its strain-specific properties such as aroma and taste), each with its own pharmacology. The cannabinoid tetrahydrocannabinol (THC) is the most widely studied and is responsible for the plant’s addictive and psychoactive effects associated with a sense of euphoria or “high,” however very few of the other cannabinoids and terpenes have been extensively studied.
Several NCCIH-funded studies are investigating the potential pain-relieving properties and mechanisms of action of substances in cannabis, including minor cannabinoids (those other than THC) and terpenes. The goal of these studies is to strengthen the evidence regarding cannabis components and whether they have potential roles in pain management. The ultimate goal of this effort is the potential development of a cannabis-based medication that maximizes its pain-relieving properties and minimizes its negative addictive and psychoactive effects.
Budget Policy:
The FY 2022 President’s Budget request for extramural basic research is $65.3 million, an increase of $13.9 million compared with the FY 2021 Enacted level.
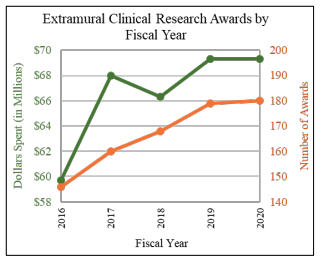
Extramural Clinical Research
The NCCIH extramural research program funds clinical investigations on complementary and integrative health practices and interventions. Projects range from small pilot studies to large-scale clinical trials and epidemiologic studies, including several collaborations between NIH Institutes and Centers and other Federal agencies. The following are recently published results from NCCIH-supported extramural clinical research.
Scientists at New York University Grossman School of Medicine and Boston University conducted a randomized, controlled, single-blind clinical trial to assess the efficacy of yoga for generalized anxiety disorder (GAD).
Cognitive behavioral therapy (CBT) is a current evidence-based psychotherapy for GAD, but many people do not receive CBT because of cost, stigma, or logistical reasons. Increasingly, people are seeking complementary interventions, such as yoga, outside the traditional medical system. The current research helps to fill in the knowledge gap on the potential benefits of yoga for GAD and how it compares to CBT. The clinical trial consisted of 230 adults with GAD that were assigned to one of three interventions: yoga, CBT, or stress management education. The researchers concluded that yoga may be a helpful, but only moderately potent intervention for GAD. However, given the increasing costs of health care and barriers to accessing trained mental health professionals, yoga may play a role in GAD management as a more easily accessible intervention. Focusing future research on identifying individual characteristics that make a person more likely to respond to yoga versus CBT could help inform how yoga might be integrated into a stepped-care personalized treatment approach to anxiety disorders.9
Researchers from the University of Michigan and Rice University examined the effect of chiropractic care accessibility on health care spending. They identified nearly 85,000 older adults enrolled in Medicare who had a spine condition and who relocated once between 2010 and 2014. They assessed the patients’ accessibility to health care for each year and estimated the effect of moving to an area of lower or higher chiropractic accessibility on spine-related spending adjusted for access to the practitioners. Although the researchers reported small differences in spending—$40 reduction in annual spending—on diagnostic imaging and tests for spine conditions, the cumulative effect could be quite large given the prevalence of spine conditions among older adults. This study is among the first to examine whether access to chiropractic care has any effect on Medicare spending. Future work may help determine if access to chiropractic care for Medicare beneficiaries in any way breaks the pathway to care that is discordant with practice guidelines.10
Budget Policy:
The FY 2022 President’s Budget request for extramural basic research is $79.9 million, an increase of $13.9 million compared with the FY 2021 Enacted level.
Intramural Research
NCCIH’s intramural research program is focused on understanding the central mechanisms of pain and its modulation, with the long-term goal of improving clinical management of chronic pain through the integration of pharmacologic and nonpharmacologic approaches. Among topics of interest are the pathways and mechanisms by which expectations, emotions, attention, environment, and genetics modulate pain or pain processing. The program both engages and leverages the exceptional basic and clinical research talent and resources of other neuroscience and neuroimaging efforts within the NIH intramural community. The following are recently published results from NCCIH intramural research.
A team of scientists have developed a new technique, using human (adult) stem cells, to efficiently grow sensory nerve cells (neurons) in a dish. This new technique allowed scientists to identify a previously unknown type of sensory neuron, which is not present in commonly used animal models. Previous research has resulted in several existing methods, using human stem cells, to grow a mixture of sensory neuron subtypes that detect different kinds of stimuli like mechanical force, cold, and heat. This new work builds on these prior techniques to precisely generate individual subtypes of sensory neurons in high purity—including a previously unrecognized class of “cold-mechanoreceptor” neuron—which the researchers suggest could be used for drug screening and studying human disorders of touch and pain. The researchers applied their new method to generate sensory neurons from human patients with a rare genetic disorder called PIEZO2 deficiency. This disorder, which was previously investigated by NIH scientists, causes a lack of the senses of touch and body position (proprioception) from birth, and it also causes insensitivity to a category of chronic pain called mechanical allodynia. Here, it was found that neurons derived from these patients are completely insensitive to mechanical stimulation, and that they can be genetically corrected using CRISPR-Cas9 to restore their sensitivity. Altogether, by producing specific neuron subtypes from individual human patients, the findings in the study emphasize how stem cells can be used to investigate human-specific aspects of sensory biology. The researchers also note that further investigation will be crucial to determine the presence of additional unrecognized sensory neuron subtypes in humans, which may not be found in commonly used animal models.11
NCCIH analyzed data from the National Ambulatory Medical Care Survey (2007–2015) for people newly diagnosed with a chronic musculoskeletal pain condition. The analysis looked at prescribed treatments at the first visit for pain. The data from 360,000 health care visits over a 9-year period indicated that many patients are initially prescribed opioids for a new chronic musculoskeletal problem. The analysis showed that opioid prescribing was double that of physical therapy. Analysts also noted that prescriptions for non-opioid medications tended to increase with patient age; opioid prescriptions peaked for patients between the ages of 25 and 64; and prescriptions for physical therapy decreased with increasing patient age. In addition, orthopedists were less likely than family practice physicians to prescribe drugs for these pain conditions, and they were more likely to prescribe physical therapy. The authors also pointed out that, per evidence-based guidelines, opioids should not be the first line of treatment, irrespective of preferences, and that opioids should not be recommended for routine management of chronic pain.12
The NIH Pain Research Center
Chronic pain affects millions of people, lacks effective treatments, and is a primary driver of opioid use disorders. Although it is a disease in its own right, pain is also associated with a wide range of medical conditions, including those found in many of the patients enrolled in studies within the NIH Clinical Center (CC). NCCIH is leading an effort to establish an intramural pain research center within the NIH CC.
The NIH Pain Research Center is an evolving, multidisciplinary, multi-Institute initiative. The mission of the Center is to create a pain classification platform within the NIH CC to better understand the mechanisms of diverse pain states in order to recommend personalized therapies to better manage or prevent the development of chronic pain. Three goals are: to identify specific pain mechanisms, to determine the efficacy of nonopioid treatments, and to predict individual patient response to therapies and outcomes. Recently, NCCIH and its NIH partners received an NIH Director’s Challenge Innovation Award to help support this center.
The NIH Pain Research Center is currently conducting 10 research studies. One project explores the question of why some patients with sickle cell disease continue to have chronic pain after reversal of sickle formation. Another delves into the question of why some people develop opioid use disorder after opioid exposure and others do not. One treatment-related study examines the use of resiniferatoxin, a natural product and nonopioid medication, for postsurgical wound pain, and another will explore the use of hydroxynorketamine for treatment of chronic pain.
As the NIH Pain Research Center grows, the hope is that it will be a nexus for NIH intramural researchers to collaborate in deciphering mechanisms underlying pain and related conditions, develop new treatment strategies, and improve patient care.
Budget Policy:
The FY 2022 President’s Budget request for NCCIH intramural research is $14.1 million, an increase of $1.3 million compared with the FY 2021 Enacted level.
Extramural Research Training and Capacity Building
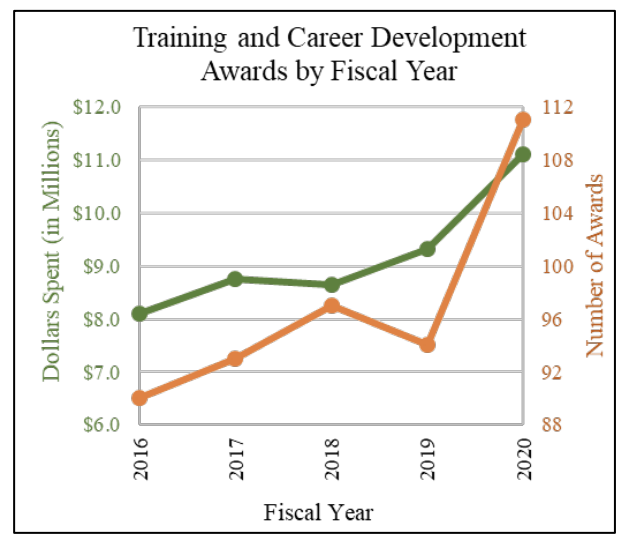
Improving the capacity of the field to carry out rigorous research on complementary and integrative health approaches is a priority for the NCCIH. To increase the number, quality, and diversity of investigators conducting this research, NCCIH supports a variety of training and career development activities for pre- and post-doctoral students, and early career investigators. NCCIH’s training strategies include innovative approaches that incorporate an understanding of the wide variety of modalities and specialization represented in complementary and integrative health field. In addition to scientists trained in key biomedical and behavioral research disciplines, the Center has opportunities for clinician-scientists, including conventionally trained physicians, complementary health practitioners, and other health care professionals (e.g., clinical psychologists, nurses) who conduct research across a wide range of complementary and integrative health approaches. NCCIH also has special opportunities for individuals from groups who are underrepresented in scientific research (e.g., racial and ethnic minority populations) and are interested in careers in complementary and integrative health research. In addition to these funding initiatives, NCCIH supports workshops to help students and fellows connect to NIH funding opportunities, understand how to interact with NIH staff to develop research proposals, navigate the NIH peer-review process successfully, develop resilience to overcome career roadblocks, and develop plans for a successful research career.
Budget Policy:
The FY 2022 President’s Budget request for extramural research training and capacity building is $4.9 million, an increase of $0.2 million compared with the FY 2021 Enacted level. This program area does not include grant awards under the Career Mechanism, which are included in extramural basic research and extramural clinical research earlier in this narrative.
Research Management Support (RMS)
Through its RMS activities, NCCIH provides administrative, budgetary, information technology, logistical, and scientific support in the review, award, monitoring, and management of research grants, training awards, and contracts. RMS functions also encompass strategic planning, coordination, and evaluation of programs. The Center uses Qlik Sense to compile interactive reports and enhanced dashboards to provide NCCIH leadership with trend data and performance indicators to ensure responsible stewardship of public funds. In addition to these activities, NCCIH disseminates objective, evidence-based information to the public, scientists, and health care providers to help them make informed decisions about the use of complementary and integrative health practices. All information is freely available on the NCCIH website (nccih.nih.gov) or through the NCCIH Information Clearinghouse.
Budget Policy:
The FY 2022 President’s Budget request for RMS is $20.2 million, an increase of $0.9 million compared with the FY 2021 Enacted level.
1Expenditures on complementary health approaches: United States, 2012. National Health Statistics Reports; no. 95, 2016. OMID: 2735222.
2Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. The Journal of Pain. 2015;16(8):769-780.
3Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Institute of Medicine, 2011.
4Stussman BJ, Nahin RL, Barnes PM, Ward BW. U.S. physician recommendations to their patients about the use of complementary health approaches. Journal of Alternative and Complementary Medicine. November 25, 2019
5Levinthal DJ and Strick PL. Multiple areas of the cerebral cortex influence the stomach. Proceedings of the National
6Yu S, Balasubramanian I, Laubitz D, et al. Paneth cell-derived lysozyme defines the composition of mucolytic microbiota and the inflammatory tone of the intestine. Immunity. 2020;53(2):398-416.
7Lai A, Ho L, Evashwick-Rogler TW, et al. Dietary polyphenols as a safe and novel intervention for modulating pain associated with intervertebral disc degeneration in an in-vivo rat model. PLoS One. 2019;14(10):e0223435.
8Ma Q, Liu S, Wand Z, et al. Somatotopic organization and intensity dependence in driving distinct NPY-expressing sympathetic pathways by electroacupuncture. Neuron. August 12, 2020.
9Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder. A randomized clinical trial. JAMA Psychiatry. 2020 Aug 12.
10Davis MA, Yakusheva O, Liu H, et al. Access to chiropractic care and the cost of spine conditions among older adults. American Journal of Managed Care. 2019;25(8):e230-e236
11Nickolls AR, Lee MM, Espinoza DF, Szczot M, Lam R, Wang Q, Beers J, Zou J, Nguyen MQ, Solinski HJ, AlJanahi AA, Johnson KR, Ward ME, Chesler AT, Bönnemann CG. Transcriptional Programming of Human Mechanosensory Neuron Subtypes from Pluripotent Stem Cells. Cell Reports. 2020
12Feldman DE, Carlesso LC, and Nahin RL. Management of patients with a musculoskeletal pain condition that is likely chronic: results from a national cross sectional survey. The Journal of Pain. 2019.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Object Class1
(Dollars in Thousands)
| FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY 2021 | |
|---|---|---|---|
| Total compensable work years: | |||
| Full-time equivalent | 79 | 90 | 11 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $0 | $0 | $0 |
| Average GM/GS grade | 13.4 | 13.4 | 0.0 |
| Average GM/GS salary | $116 | $119 | $3 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $142 | $146 | $4 |
| Average salary of ungraded positions | $198 | $203 | $6 |
| OBJECT CLASSES | FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY 2021 |
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | 7,368 | 7,762 | 394 |
| 11.3 Other Than Full-Time Permanent | 2,466 | 2,690 | 224 |
| 11.5 Other Personnel Compensation | 387 | 407 | 20 |
| 11.7 Military Personnel | 204 | 237 | 32 |
| 11.8 Special Personnel Services Payments | 1,036 | 1,256 | 220 |
| 11.9 Subtotal Personnel Compensation | $11,461 | $12,351 | $890 |
| 12.1 Civilian Personnel Benefits | 4,055 | 4,430 | 375 |
| 12.2 Military Personnel Benefits | 137 | 159 | 22 |
| 13.0 Benefits to Former Personnel | 0 | 0 | 0 |
| Subtotal Pay Costs | $15,653 | $16,940 | $1,287 |
| 21.0 Travel & Transportation of Persons | 121 | 380 | 259 |
| 22.0 Transportation of Things | 10 | 10 | 0 |
| 23.1 Rental Payments to GSA | 19 | 20 | 0 |
| 23.2 Rental Payments to Others | 0 | 0 | 0 |
| 23.3 Communications, Utilities & Misc. Charges | 80 | 82 | 1 |
| 24.0 Printing & Reproduction | 3 | 3 | 0 |
| 25.1 Consulting Services | 4,749 | 4,939 | 191 |
| 25.2 Other Services | 1,995 | 2,031 | 36 |
| 25.3 Purchase of goods and services from government accounts | 13,929 | 14,739 | 810 |
| 25.4 Operation & Maintenance of Facilities | 2 | 2 | 0 |
| 25.5 R&D Contracts | 4,491 | 5,158 | 667 |
| 25.6 Medical Care | 102 | 106 | 4 |
| 25.7 Operation & Maintenance of Equipment | 199 | 202 | 4 |
| 25.8 Subsistence & Support of Persons | 0 | 0 | 0 |
| 25.0 Subtotal Other Contractual Services | $25,466 | $27,177 | $1,711 |
| 26.0 Supplies & Materials | 396 | 403 | 7 |
| 31.0 Equipment | 921 | 937 | 17 |
| 32.0 Land and Structures | 0 | 0 | 0 |
| 33.0 Investments & Loans | 0 | 0 | 0 |
| 41.0 Grants, Subsidies & Contributions | 111,410 | 138,371 | 26,961 |
| 42.0 Insurance Claims & Indemnities | 0 | 0 | 0 |
| 43.0 Interest & Dividends | 0 | 0 | 0 |
| 44.0 Refunds | 0 | 0 | 0 |
| Subtotal Non-Pay Costs | $138,426 | $167,383 | $28,957 |
| Total Budget Authority by Object Class | $154,079 | $184,323 | $30,244 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2021 Enacted | FY 2022 President’s Budget | FY 2022 +/- FY 2021 |
|---|---|---|---|
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $7,368 | $7,762 | $394 |
| Other Than Full-Time Permanent (11.3) | 2,466 | 2,690 | 224 |
| Other Personnel Compensation (11.5) | 387 | 407 | 20 |
| Military Personnel (11.7) | 204 | 237 | 32 |
| Special Personnel Services Payments (11.8) | 1,036 | 1,256 | 220 |
| Subtotal Personnel Compensation (11.9) | $11,461 | $12,351 | $890 |
| Civilian Personnel Benefits (12.1) | $4,055 | $4,430 | $376 |
| Military Personnel Benefits (12.2) | 137 | 159 | 22 |
| Benefits to Former Personnel (13.0) | 0 | 0 | 0 |
| Subtotal Pay Costs | $15,653 | $16,940 | $1,287 |
| Travel & Transportation of Persons (21.0) | $121 | $380 | $259 |
| Transportation of Things (22.0) | 10 | 10 | 0 |
| Rental Payments to Others (23.2) | 0 | 0 | 0 |
| Communications, Utilities & Misc. Charges (23.3) | 80 | 82 | 1 |
| Printing & Reproduction (24.0) | 3 | 3 | 0 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | 4,749 | 4,939 | 191 |
| Other Services (25.2) | 1,995 | 2,031 | 36 |
| Purchases from government accounts (25.3) | 9,944 | 10,423 | 479 |
| Operation & Maintenance of Facilities (25.4) | 2 | 2 | 0 |
| Operation & Maintenance of Equipment (25.7) | 199 | 202 | 4 |
| Subsistence & Support of Persons (25.8) | 0 | 0 | 0 |
| Subtotal Other Contractual Services | $16,888 | $17,598 | $709 |
| Supplies & Materials (26.0) | $396 | $403 | $7 |
| Subtotal Non-Pay Costs | $17,498 | $18,475 | $977 |
| Total Administrative Costs | $33,151 | $35,415 | $2,264 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Full-Time Equivalent Employment (FTE)
| OFFICE/DIVISION | FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Office of Scientific Review | |||||||||
| Direct: | 4 | - | 4 | 4 | - | 4 | 5 | - | 5 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 4 | - | 4 | 4 | - | 4 | 5 | - | 5 |
| Division of Extramural Activities | |||||||||
| Direct: | 3 | - | 3 | 4 | - | 4 | 4 | - | 4 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 3 | - | 3 | 4 | - | 4 | 4 | - | 4 |
| Division of Extramural Research | |||||||||
| Direct: | 16 | - | 16 | 17 | - | 17 | 19 | - | 19 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 16 | - | 16 | 17 | - | 17 | 19 | - | 19 |
| Division of Intramural Research Program | |||||||||
| Direct: | 7 | 1 | 8 | 10 | 1 | 11 | 13 | 1 | 14 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 7 | 1 | 8 | 10 | 1 | 11 | 13 | 1 | 14 |
| Office of Administrative Operations | |||||||||
| Direct: | 14 | - | 14 | 17 | - | 17 | 19 | - | 19 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 14 | - | 14 | 17 | - | 17 | 19 | - | 19 |
| Office of Clinical and Regulatory Affairs | |||||||||
| Direct: | 5 | - | 5 | 4 | - | 4 | 6 | - | 6 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 5 | - | 5 | 4 | - | 4 | 6 | - | 6 |
| Office of Communications and Public Liaison | |||||||||
| Direct: | 9 | - | 9 | 9 | - | 9 | 10 | - | 10 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 9 | - | 9 | 9 | - | 9 | 10 | - | 10 |
| Office of Grants Management | |||||||||
| Direct: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 3 | - | 3 | 3 | - | 3 | 3 | - | 3 |
| Office of Policy, Planning, and Evaluation | |||||||||
| Direct: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 4 | - | 4 | 4 | - | 4 | 4 | - | 4 |
| Office of the Director | |||||||||
| Direct: | 5 | - | 5 | 6 | - | 6 | 6 | - | 6 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 5 | - | 5 | 6 | - | 6 | 6 | - | 6 |
| Total | 70 | 1 | 71 | 78 | 1 | 79 | 89 | 1 | 90 |
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FISCAL YEAR | Average GS Grade | ||||||||
| 2018 | 12.8 | ||||||||
| 2019 | 13.2 | ||||||||
| 2020 | 13.3 | ||||||||
| 2021 | 13.4 | ||||||||
| 2022 | 13.4 | ||||||||
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Positions1
| GRADE | FY 2020 Final | FY 2021 Enacted | FY 2022 President’s Budget |
|---|---|---|---|
| Total, ES Positions | 0 | 0 | 0 |
| Total, ES Salary General Schedule | 0 | 0 | 0 |
| GM/GS-15 | 13 | 13 | 14 |
| GM/GS-14 | 16 | 15 | 17 |
| GM/GS-13 | 20 | 18 | 20 |
| GS-12 | 10 | 13 | 15 |
| GS-11 | 5 | 4 | 6 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 0 | 1 | 2 |
| GS-8 | 0 | 0 | 0 |
| GS-7 | 1 | 1 | 1 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 0 | 0 | 0 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 65 | 65 | 75 |
| Commissioned Corps (42 U.S.C. 207) | |||
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 1 | 1 | 1 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 1 | 1 | 1 |
| Ungraded | 29 | 29 | 30 |
| Total permanent positions | 64 | 72 | 83 |
| Total positions, end of year | 95 | 95 | 106 |
| Total full-time equivalent (FTE) employment, end of year | 71 | 79 | 90 |
| Average ES salary | 0 | 0 | 0 |
| Average GM/GS grade | 13.3 | 13.4 | 13.4 |
| Average GM/GS salary | 112,397 | 115,544 | 118,779 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||