Congressional Justification FY 2023
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health (NCCIH)
On this page:
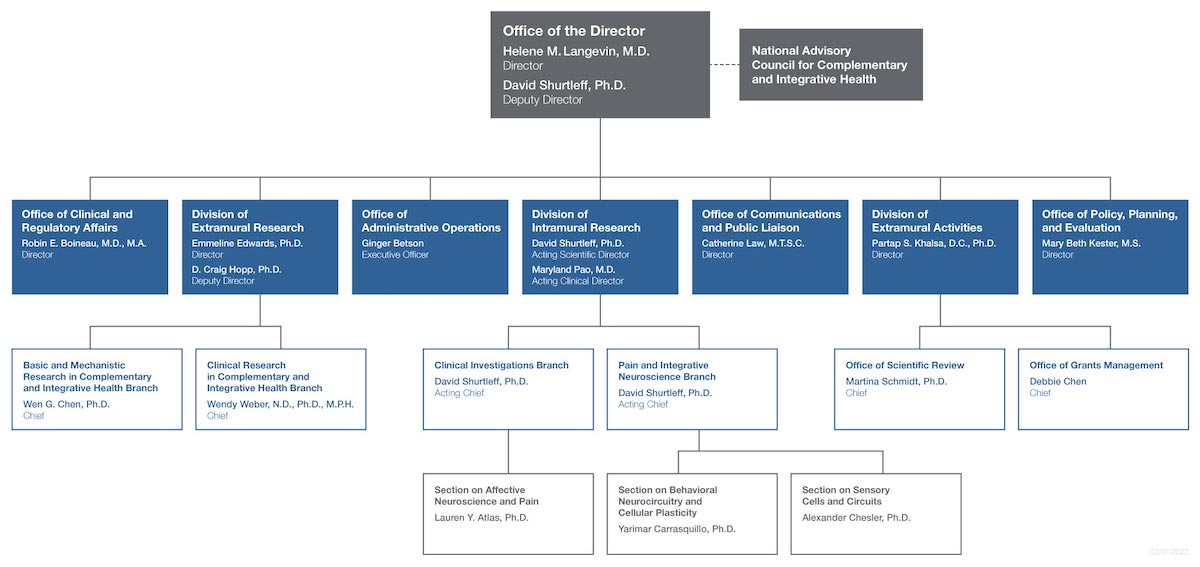
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Mechanism Table
- Major Changes in Budget Request
- Summary of Changes
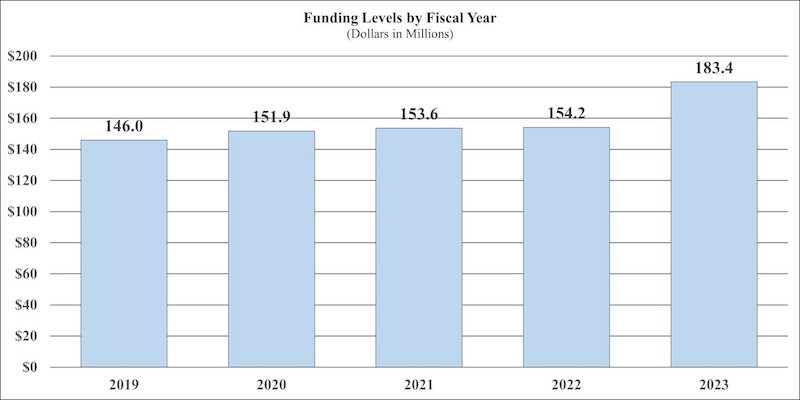
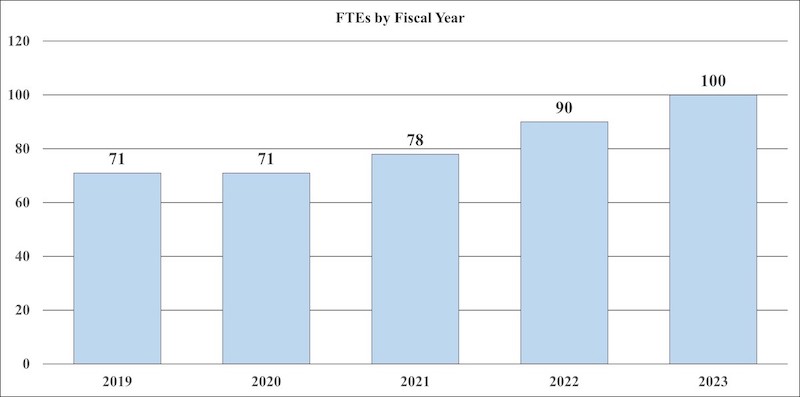
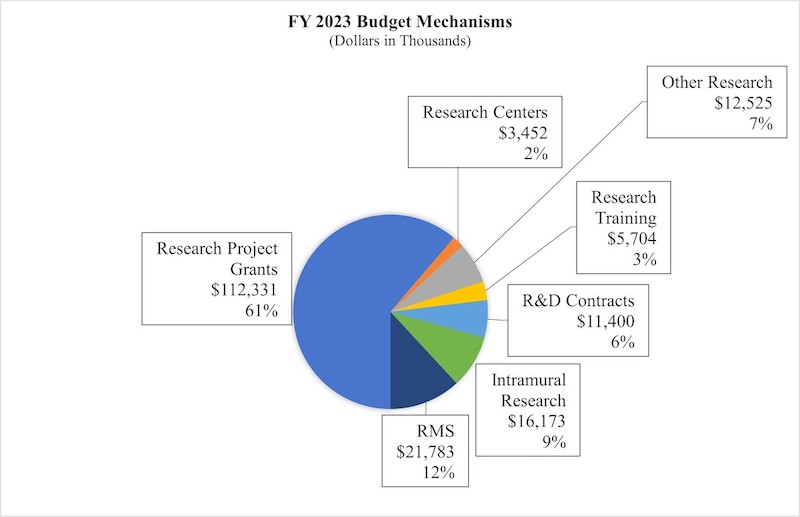
- Budget Graphs
- Budget Authority by Activity
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
NATIONAL INSTITUTES OF HEALTH
NATIONAL CENTER FOR COMPLEMENTARY AND INTEGRATIVE HEALTH
For carrying out section 301 and title IV of the PHS Act with respect to complementary and integrative health, $183,368,000.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Amounts Available for Obligation 1
(Dollars in Thousands)
| Source of Funding | FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget |
|---|---|---|---|
| Appropriation | $154,162 | $154,162 | $183,368 |
| Mandatory Appropriation: (non-add) | |||
| Type 1 Diabetes | ($0) | ($0) | ($0) |
| Other Mandatory financing | ($0) | ($0) | ($0) |
| Secretary's Transfer | -$463 | $0 | $0 |
| Subtotal, adjusted appropriation | $153,699 | $154,162 | $183,368 |
| OAR HIV/AIDS Transfers | -$83 | $0 | $0 |
| Subtotal, adjusted budget authority | $153,616 | $154,162 | $183,368 |
| Unobligated balance, start of year | $0 | $0 | $0 |
| Unobligated balance, end of year (carryover) | $0 | $0 | $0 |
| Subtotal, adjusted budget authority | $153,616 | $154,162 | $183,368 |
| Unobligated balance lapsing | -$15 | $0 | $0 |
| Total obligations | $153,601 | $154,162 | $183,368 |
| 1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2021 — $1,466 FY 2022 — $1,390 FY 2023 — $1,140 | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Mechanism - Total 1
(Dollars in Thousands)
| MECHANISM | FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 CR | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 121 | $66,924 | 118 | $65,270 | 112 | $61,705 | -6 | $3,565 |
| Administrative Supplements | (25) | 2,996 | (8) | 950 | (8) | 950 | (0) | 0 |
| Competing: | ||||||||
| Renewal | 1 | 600 | 1 | 459 | 0 | 0 | -1 | -459 |
| New | 44 | 18,747 | 35 | 14,667 | 80 | 44,437 | 45 | 29,770 |
| Supplements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Subtotal, Competing | 45 | $19,347 | 36 | $15,125 | 80 | $44,437 | 44 | $29,312 |
| Subtotal, RPGs | 166 | $89,268 | 154 | $81,345 | 192 | $107,091 | 38 | $25,746 |
| SBIR/STTR | 8 | 4,381 | 9 | 4,308 | 11 | 5,239 | 2 | 931 |
| Research Project Grants | 174 | $93,649 | 163 | $85,653 | 203 | $112,331 | 40 | $26,677 |
| Research Centers: | ||||||||
| Specialized/Comprehensive | 1 | $2,596 | 2 | $3,294 | 2 | $3,452 | 0 | $159 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 1 | 733 | 0 | 0 | 0 | 0 | 0 | 0 |
| Comparative Medicine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers in Minority Institutions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers | 2 | $3,328 | 2 | $3,294 | 2 | $3,452 | 0 | $159 |
| Other Research: | ||||||||
| Research Careers | 36 | $5,832 | 35 | $5,681 | 27 | $4,391 | -8 | $1,290 |
| Cancer Education | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cooperative Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Minority Biomedical Research Support | 0 | 150 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 9 | 5,439 | 15 | 9,158 | 13 | 8,134 | -2 | -1,023 |
| Other Research | 45 | $11,421 | 50 | $14,838 | 40 | $12,525 | -10 | -$2,313 |
| Total Research Grants | 221 | $108,399 | 215 | $103,785 | 245 | $128,308 | 30 | $24,523 |
| Ruth L Kirchstein Training Awards: | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 20 | $855 | 20 | $876 | 21 | $919 | 1 | $43 |
| Institutional Awards | 46 | 3,774 | 49 | 3,997 | 58 | 4,784 | 9 | 788 |
| Total Research Training | 66 | $4,629 | 69 | $4,873 | 79 | $5,704 | 10 | $831 |
| Research & Develop. Contracts | 10 | $8,563 | 14 | $11,176 | 14 | $11,400 | 0 | $224 |
| (SBIR/STTR) (non-add) | (0) | (46) | (0) | (45) | (0) | (55) | (0) | (10) |
| Intramural Research | 11 | 12,785 | 12 | 14,703 | 16 | 16,173 | 4 | 1,470 |
| Res. Management & Support | 67 | 19,240 | 78 | 19,625 | 84 | 21,783 | 6 | 2,159 |
| SBIR Admin (non-add) | (0) | (66) | (0) | (0) | (0) | (0) | (0) | (0) |
| Construction | 0 | 0 | 0 | 0 | ||||
| Buildings and Facilities | 0 | 0 | 0 | 0 | ||||
| Total, NCCIH | 78 | $153,616 | 90 | $154,162 | 100 | $183,368 | 10 | $29,206 |
1 All items in italics and brackets are non-add entries.
Major Changes in the Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanisms and activity detail, and these highlights will not sum to the total change for the FY 2023 budget request for the NCCIH, which is $183.4 million, an increase of $29.2 million from the FY 2022 CR level. Within the request level, NCCIH will pursue its highest research priorities through strategic investments and careful stewardship of appropriated funds.
Research Project Grants (+$26.7 million; total $112.3 million): NCCIH will support a total of 203 Research Project Grant (RPG) awards in FY 2023. Noncompeting RPGs will decrease by $3.6 million, while Competing RPG awards will increase by $29.3 million.
R&D Contracts (+$0.2 million; total $11.4 million): NCCIH will continue its annual support to the National Health Interview Survey (NHIS) and other mission-supporting Research and Development Contracts.
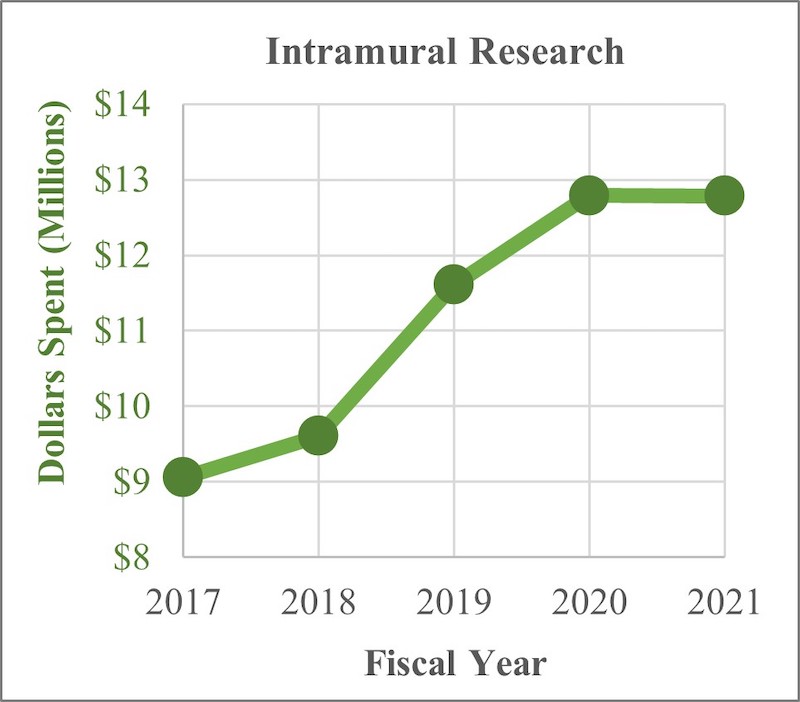
Intramural Research (+$1.5 million; total $16.2 million): NCCIH will continue to support intramural research activities, including the NIH Pain Research Center.
Research Management and Support (+$2.2 million; total $21.8 million): NCCIH will manage a full-time equivalent staff level of 100 and fund the costs of pay raises, benefit increases, and other inflation.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Summary of Changes
(Dollars in Thousands)
| FY 2022 CR | $154,162 | ||||||
|---|---|---|---|---|---|---|---|
| FY 2023 President’s Budget | $183,368 | ||||||
| Net Change | $29,206 | ||||||
| CHANGES | FY 2022 CR | FY 2023 President’s Budget | Built-In Change from FY 2022 CR | ||||
| FTEs | Budget Authority | FTEs | Budget Authority | FTEs | Budget Authority | ||
| A. Built-in: | |||||||
| 1. Intramural Research: | |||||||
| a. Annualization of January 2022 pay increase & benefits | $3,943 | $4,520 | $26 | ||||
| b. January FY 2023 pay increase & benefits | 3,943 | 4,520 | 133 | ||||
| c. Paid days adjustment | 3,943 | 4,520 | -15 | ||||
| d. Differences attributable to change in FTE | 3,943 | 4,520 | 1,314 | ||||
| e. Payment for centrally furnished services | 1,924 | 2,159 | 236 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 8,836 | 9,494 | 195 | ||||
| Subtotal | $1,889 | ||||||
| 2. Research Management and Support: | |||||||
| a. Annualization of January 2022 pay increase & benefits | $13,322 | $15,184 | $88 | ||||
| b. January FY 2023 pay increase & benefits | 13,322 | 15,184 | 449 | ||||
| c. Paid days adjustment | 13,322 | 15,184 | -51 | ||||
| d. Differences attributable to change in FTE | 13,322 | 15,184 | 1,052 | ||||
| e. Payment for centrally furnished services | 428 | 485 | 57 | ||||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 5,875 | 6,114 | 129 | ||||
| Subtotal | $1,724 | ||||||
| Subtotal, Built-in | $3,613 | ||||||
| CHANGES | FY 2022 CR | FY 2023 President’s Budget | Program Change from FY 2022 CR | |||
|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 118 | $66,220 | 112 | $62,655 | -6 | -$3,565 |
| b. Competing | 36 | 15,125 | 80 | 44,437 | 44 | 29,312 |
| c. SBIR/STTR | 9 | 4,308 | 11 | 5,239 | 2 | 931 |
| Subtotal, RPGs | 163 | $85,653 | 203 | $112,331 | 40 | $26,677 |
| 2. Research Centers | 2 | $3,294 | 2 | $3,452 | 0 | $159 |
| 3. Other Research | 50 | 14,838 | 40 | 12,525 | -10 | -2,313 |
| 4. Research Training | 69 | 4,873 | 79 | 5,704 | 10 | 831 |
| 5. Research and development contracts | 14 | 11,176 | 14 | 11,400 | 0 | $224 |
| Subtotal, Extramural | $119,834 | $145,411 | $25,577 | |||
| 6. Intramural Research | 12 | $14,703 | 16 | $16,173 | 4 | -$419 |
| 7. Research Management and Support | 78 | 19,625 | 84 | 21,783 | 6 | 435 |
| 8. Construction | 0 | 0 | 0 | |||
| 9. Buildings and Facilities | 0 | 0 | 0 | |||
| Subtotal, Program | 90 | $154,162 | 100 | $183,368 | 10 | $25,593 |
| Total built-in and program changes | $29,206 | |||||
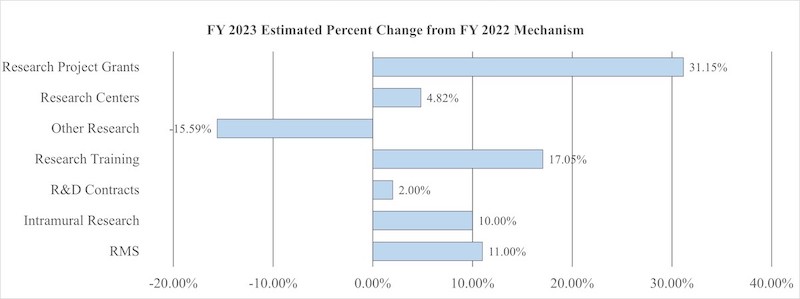
Fiscal Year 2023 Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanisms:
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Activity1
(Dollars in Thousands)
| FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY2022 CR | |||||
|---|---|---|---|---|---|---|---|---|
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | ||||||||
| Detail | ||||||||
| Clinical Research-Non Pain | $40,433 | $39,760 | $40,587 | $827 | ||||
| Basic Research-Non Pain | 29,971 | 29,472 | 28,681 | -791 | ||||
| Extramural Pain and Pain Management | 40,726 | 40,048 | 66,048 | 26,000 | ||||
| Extramural Research Training and Capacity Building | 10,461 | 10,554 | 10,094 | -459 | ||||
| Subtotal, Extramural | $121,591 | $119,834 | $145,411 | $25,577 | ||||
| Intramural Research | 11 | $12,785 | 12 | $14,703 | 16 | $16,173 | 4 | $1,470 |
| Research Management & Support | 67 | $19,240 | 78 | $19,625 | 84 | $21,783 | 6 | $2,159 |
| TOTAL | 78 | $153,616 | 90 | $154,162 | 100 | $183,368 | 10 | $29,206 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2022 Amount Authorized | FY 2022 CR | 2023 Amount Authorized | FY 2023 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | Indefinite | ||||
| $154,162,000 | $183,368,000 | |||||||
| National Center for Complementary and Integrative Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total, Budget Authority | $154,162,000 | $183,368,000 | ||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation | ||||
|---|---|---|---|---|---|---|---|---|
1 Budget Estimate to Congress includes mandatory financing. | ||||||||
| 2014 | $129,041,000 | $128,183,000 | $124,296,000 | |||||
| Rescission | $0 | |||||||
| 2015 | $124,509,000 | $124,681,000 | ||||||
| Rescission | $0 | |||||||
| 2016 | $127,521,000 | $127,585,000 | $130,162,000 | $130,789,000 | ||||
| Rescission | $0 | |||||||
| 20171 | $129,941,000 | $134,549,000 | $136,195,000 | $134,689,000 | ||||
| Rescission | $0 | |||||||
| 2018 | $101,793,000 | $136,741,000 | $139,654,000 | $142,184,000 | ||||
| Rescission | $0 | |||||||
| 2019 | $130,717,000 | $143,882,000 | $146,550,000 | $146,473,000 | ||||
| Rescission | $0 | |||||||
| 2020 | $126,081,000 | $153,632,000 | $154,695,000 | $151,740,000 | ||||
| Rescission | $0 | |||||||
| 2021 | $138,167,000 | $153,045,000 | $156,823,000 | $154,162,000 | ||||
| Rescission | $0 | |||||||
| 2022 | $184,323,000 | $185,295,000 | $184,249,000 | $154,162,000 | ||||
| Rescission | $0 | |||||||
| 2023 | $183,368,000 | |||||||
Justification of Budget Request
National Center for Complementary and Integrative Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 | |
|---|---|---|---|---|
| BA | $153,616,000 | $154,162,000 | $183,368,000 | +$29,206,000 |
| FTE | 78 | 90 | 100 | +10 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2023 President’s Budget request for NCCIH is $183.4 million, an increase of $29.2 million or 18.9 percent above the FY 2022 CR level. $26.0 million of this increase will be allocated to expanding NCCIH research into pain and pain management.
Director's Overview
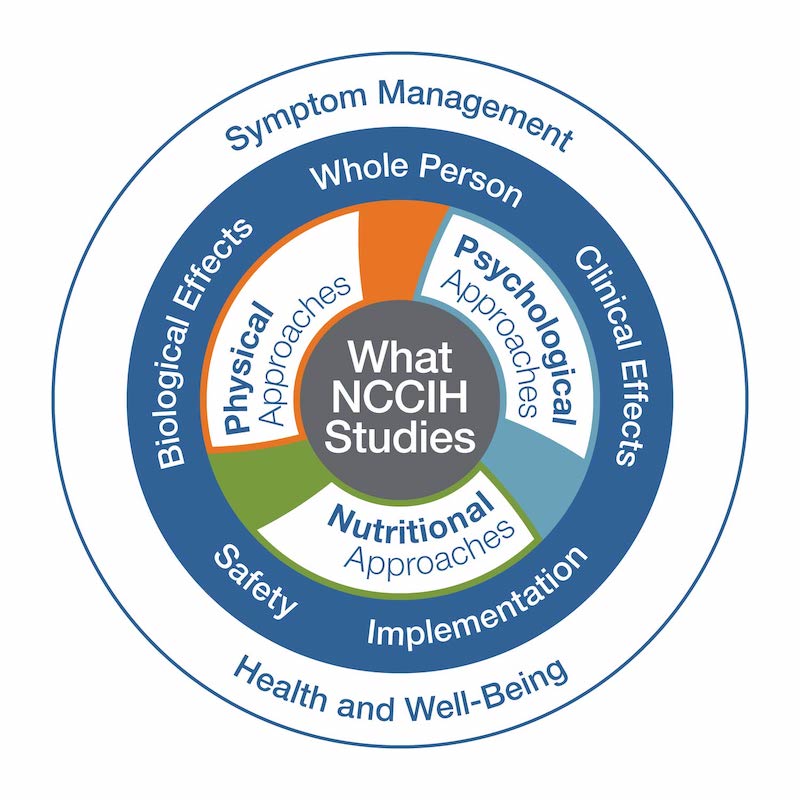
The mission of the National Center for Complementary and Integrative Health (NCCIH) is to define, through rigorous scientific investigation, the fundamental mechanisms, usefulness, and safety of complementary and integrative health approaches and their roles in improving health and health care.
Americans spend approximately $30.2 billion per year on complementary health treatments, practices, and products.1 This diverse group of health practices includes nutritional, psychological, and physical approaches that may have originated outside of conventional medicine. These include natural products, such as dietary supplements, plant-based products, and probiotics, as well as mind and body approaches, such as yoga, massage therapy, meditation, mindfulness-based stress reduction, spinal manipulation, and acupuncture. These treatment and self-care options are typically used in conjunction with conventional medicine to promote health and well-being, manage symptoms of a disease or condition, or alleviate side effects of medications. Integrative health care seeks to bring conventional and complementary approaches together in a safe, coordinated way with the goal of improving clinical care for patients, restoring health, promoting resilience, and preventing disease.
During the last few years, NCCIH has continued to expand research efforts around pain and pain management. The Center supported research on natural products for pain management, including cannabinoids and terpenes. The Center funded a large-scale, multisite, multicomponent clinical trial investigating the use of spinal manipulation and patient self-management to prevent back pain chronicity. Finally, the Center continued support of the National Institutes of Health (NIH)–Department of Defense (DoD)–Department of Veterans Affairs (VA) Pain Management Collaboratory.
As a responsible steward of resources, we are highly selective and support a broad range of scientifically meritorious basic, mechanistic, clinical, translational, dissemination, and implementation research. We focus on areas with the greatest impact by prioritizing research topics that show scientific promise and are amenable to rigorous scientific inquiry. We strive to invest in research that will drive new discoveries and may lead to improved public health and health care. The following are some of our recent efforts to respond to the ever-changing world and to enhance human health and well-being.
The importance of complementary and integrative health approaches during a pandemic
As the COVID-19 pandemic continues to take lives around the world, the social distancing measures put in place to stop the spread of the SARS-CoV-2 virus have profoundly affected daily life, shutting down businesses, schools, and cities, adding to the stress caused by illness and grief. As the stress and social isolation of the pandemic took a toll on the population, complementary and integrative health approaches were uniquely positioned to help. Many complementary and integrative health practices, such as yoga, mindfulness meditation, and basic relaxation techniques, can help promote resilience during stressful or adverse life events. The ability to implement these practices into self-care routines at home makes them ideal during a socially isolated pandemic. In response to the pandemic, NCCIH worked to expand research related to behavioral interventions for stress management, evaluate natural products for the treatment and management of COVID-19, and improve digital health care interventions (e.g., mobile health [mHealth], telemedicine and telehealth, health information technology [IT], and wearable devices) for long-distance treatment and self-care. The Center supported research to improve the understanding, prevention, and treatment of “long COVID,” a condition characterized by prolonged COVID-19 symptoms. In addition to these efforts, the NCCIH Office of Communications and Public Liaison worked to dispel misinformation about dangerous and ineffective alternative medicine approaches for the treatment or prevention of COVID-19.
The COVID-19 pandemic also highlighted a need for research that focuses on health and the whole person. For example, although COVID-19 is a respiratory infection, chronic conditions in other body systems are important factors in its severity and mortality and, layered with socioeconomic factors, serve to exacerbate the burden of COVID-19. COVID-19 may be the first major pandemic of our lifetime, but Americans have been facing the realities of “non-communicable epidemics” for some time—opioid abuse, chronic pain, obesity, diabetes, and suicide. As a nation, the United States is in an alarmingly poor overall state of health. This situation manifests in the decline in life expectancy and the prevalence of multiple chronic conditions in individuals, such as obesity, diabetes, cardiovascular disease, and degenerative joint disease. Many of these chronic diseases are not only linked to chronic pain and COVID-19 severity but also share common roots, such as poor diet, sedentary lifestyle, and chronic stress. Now, more than ever, there is a need to look at the multiple factors that promote either health or disease and scientifically consider the whole person as a complex system in which health and disease are part of a bidirectional continuum.
The current biomedical research model is superb in advancing the diagnosis and pharmacologic treatment of organ-specific diseases with growing precision. This knowledge is based on an increasingly sophisticated understanding of pathogenesis—the mechanisms by which diseases occur. On the other hand, health restoration through self-care, lifestyle, or behavioral interventions is much less studied. This is a new area of focus for NCCIH, which is referred to as research on whole person health and is highlighted in our most recent strategic plan. Research on whole person health focuses on health as a biopsychosocial process that involves the whole person. By deepening our scientific understanding of the connections that exist across domains of human health, we can better understand how conditions interrelate, define multicomponent interventions that address these problems, and improve how we support patients through the full continuum of their health experience, including the return to health.
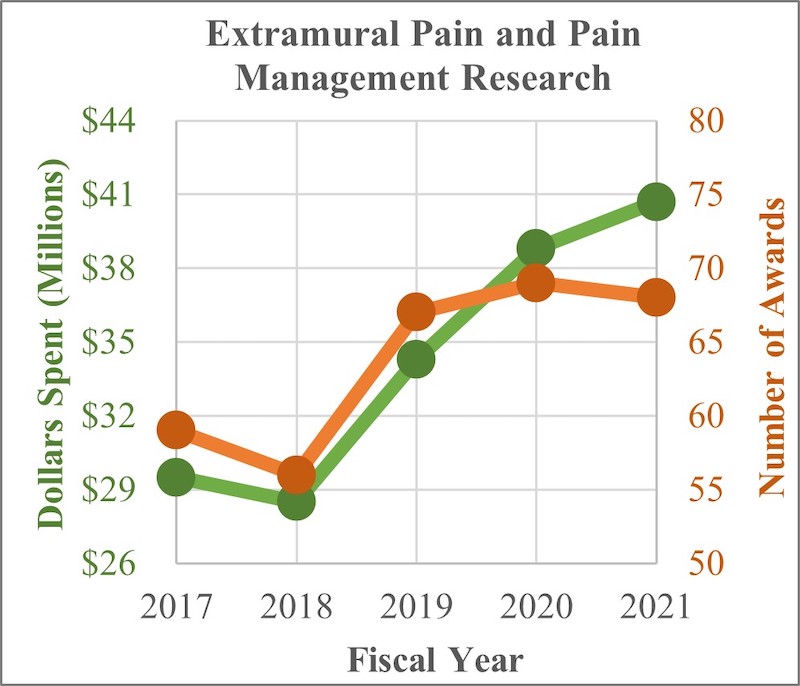
The pain and opioid misuse epidemic
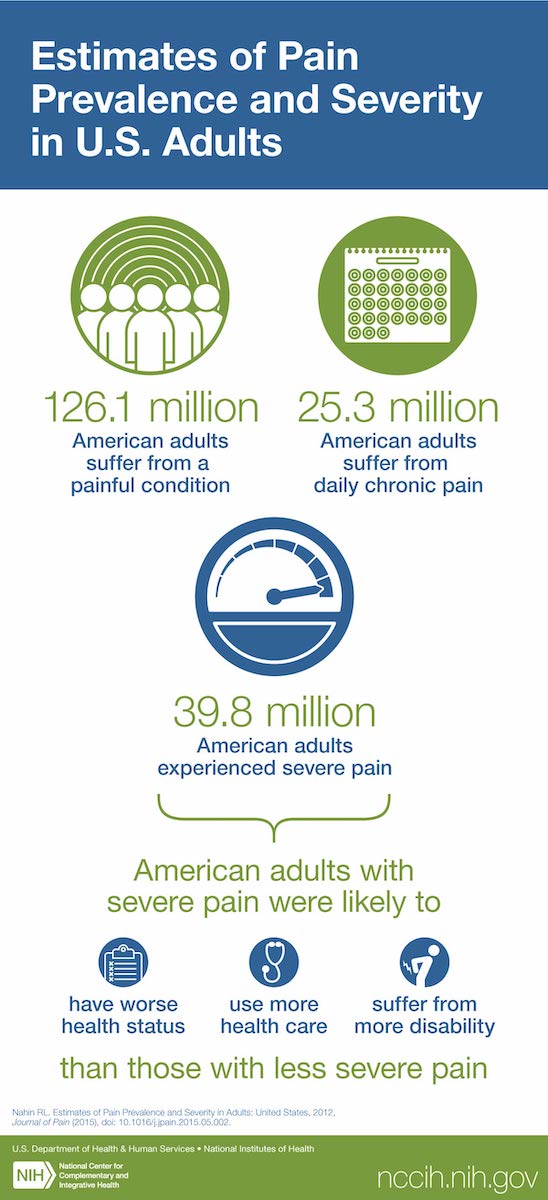
Pain is a major public health problem and is the most common reason why Americans use complementary and integrative health practices. Chronic pain affects millions of people, lacks effective treatments, and is a primary driver of opioid use disorders. There is an urgent need for nonaddictive approaches that can relieve or reduce pain and increase functional ability. NCCIH has taken on this challenge by investing heavily in pain and pain management research.
The Center’s Intramural Research Program conducts basic, clinical, and translational research focusing on the role of the brain in perceiving, modifying, and managing pain. NCCIH is also leading an effort to establish and maintain an intramural pain research center within the NIH Clinical Center. The NIH Pain Research Center is an evolving, multidisciplinary, multi-Institute initiative. Its mission is to better understand the mechanisms of diverse pain states to recommend personalized therapies to better manage or prevent the development of chronic pain.
Through its Extramural Research Program, NCCIH supports pain and pain management research across the clinical pipeline from basic and mechanistic research through dissemination and implementation research. These efforts focus on understanding the basic biology of pain, identifying novel natural products for pain management, optimizing behavioral approaches to manage pain and opioid cravings, evaluating pain management options in real-world settings, and improving the implementation of evidence-based practices.
NCCIH Framework for Clinical Research
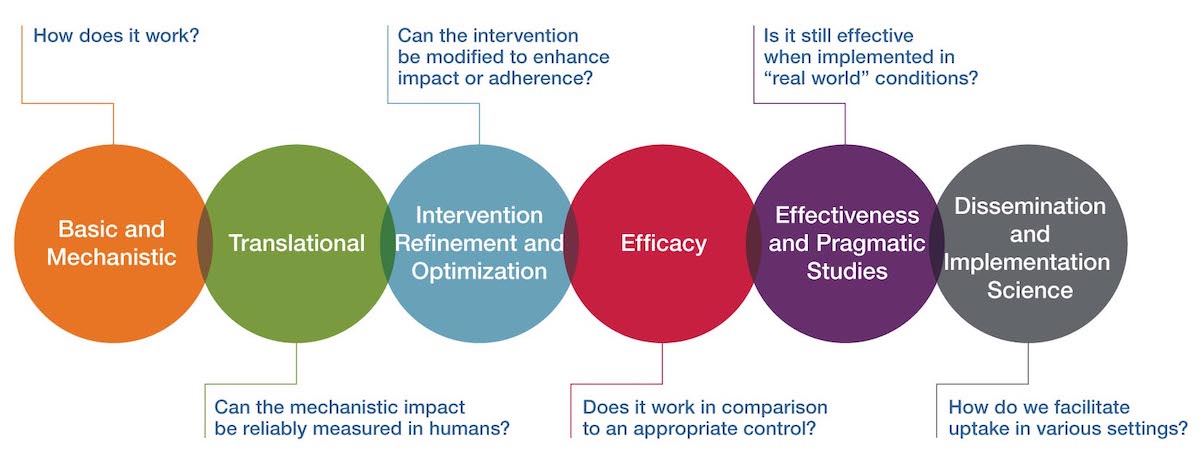
Efforts related to dissemination and implementation research
The focus of research that NCCIH supports is the use of science to enhance and maintain human health through complementary and integrative health approaches. It is important that the lessons learned from this research are relevant to inform and improve the quality of health, delivery of services, and utilization and sustainability of evidence-based treatment options. For many years, it has been assumed that tools and interventions deemed efficacious within clinical or community-based trials would be readily adopted and implemented; however, compelling evidence suggests that this has not been the case. This is true across all biomedical specialties, not just complementary and integrative health. NCCIH is seeking to remedy the gap between research and treatment by investing in dissemination and implementation research. Dissemination research seeks to understand how best to spread and sustain knowledge about cutting-edge, evidence-based interventions. Implementation science seeks to understand why efficacious tools and interventions are not being adopted and how those barriers can be overcome. NCCIH has made dissemination and implementation research a high scientific priority. The goals of this effort are to facilitate the uptake and adoption of evidence-based complementary and integrative health approaches, to advance the fields of dissemination and implementation science, and to increase awareness of the importance of dissemination and implementation research. NCCIH plans to accomplish this goal through targeted stakeholder outreach, expanded funding opportunities, and updated messaging. The following are some of the efforts the Center has undertaken in this area.
In 2019, NCCIH convened an expert panel to discuss implementation methodologies and potential paths forward. The panel identified many factors that can impact the implementation of evidence-based interventions. These include insurance coverage, patient expectations, physician recommendations, cultural background, and intervention availability. This meeting identified the landscape of issues to be addressed for successful implementation of evidence-based practices and has helped shape the Center’s strategies for advancing this area of science.
NCCIH is working to support research that evaluates hurdles to the dissemination and implementation of evidence-based practices and develops strategies to pass them. The Center has released funding opportunities specific to these issues. In addition, NCCIH expanded pragmatic clinical research initiatives such as the NIH Health Care Systems Research Collaboratory, the Pragmatic and Implementation Studies for the Management of Pain to Reduce Opioid Prescribing (PRISM), and the NIH-DoD-VA Pain Management Collaboratory to include dissemination and implementation research. The hope is that research supported by these initiatives will increase uptake of evidence-based treatments by engaging policymakers, payers, health care providers, and patients across diverse patient care settings.
In addition to new funding opportunities, NCCIH has worked to communicate the importance of dissemination and implementation research. The Center published a scientific review article on the topic, included dissemination and implementation research as a scientific priority in its most recent strategic plan, and added dissemination and implementation research to its framework for clinical research. These moves were intended to highlight the importance of this area of research and to encourage investigators to think about implementation at the beginning of a study.
Program Descriptions
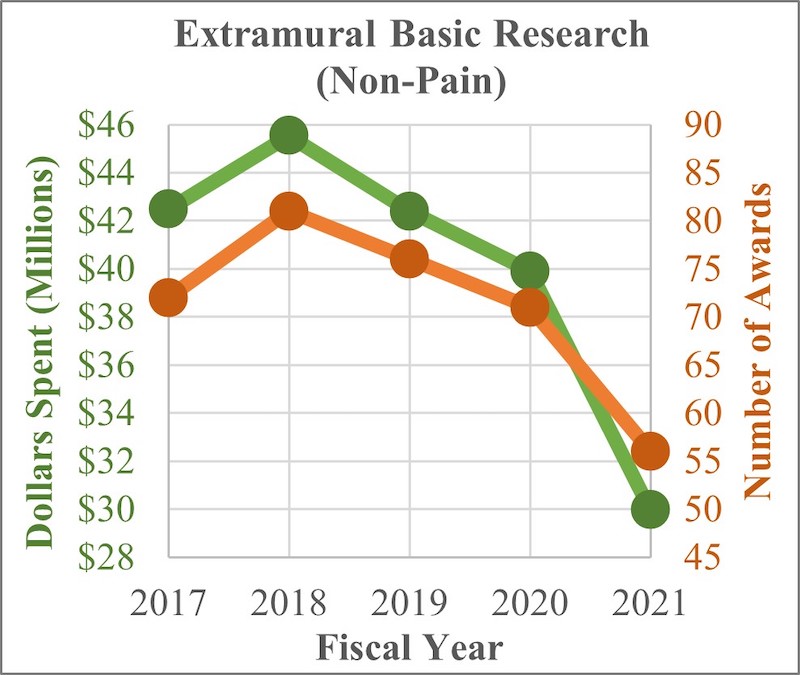
Extramural Basic Research (Not Pain Related)

The NCCIH extramural basic research program seeks to understand the fundamental science of complementary health approaches such as their biology, physiology, and physical, chemical, and behavioral properties. This includes research on basic physiological and pathophysiological mechanisms relevant to complementary and integrative health. It also includes identifying and understanding the active components of a complementary health approach and how these components produce effects. Depending on the question, basic and mechanistic studies may be performed in the laboratory, in experimental models, or with research participants. NCCIH is also energizing the research community to overcome the methodologic and technologic obstacles hindering basic research on natural products and nonpharmacologic therapies, as well as encouraging the incorporation of cutting-edge technologies to monitor and enhance these interventions. The following is an example of research supported by this program.
Researchers from the Massachusetts Institute of Technology and the Salk Institute for Biological Studies evaluated how social isolation impacts the brain and how that compares to hunger. The researchers used functional magnetic resonance imaging (fMRI) to monitor brain activity following 10 hours of social isolation or fasting. They found similarities in the brain’s craving responses to social isolation and hunger. Specifically, a small structure in the midbrain called the substantia nigra pars compacta and ventral tegmental area (SN/VTA) responded to both food cues after fasting and social cues after isolation. The SN/VTA consists mostly of dopaminergic neurons, which are nerve cells that create and release the brain chemical dopamine. In other parts of the brain, including the striatal and cortical regions, neural responses differed between craving food and craving social interaction. Both fasting and social isolation narrowed and focused the brain’s motivational response to the specific type of deprivation. The finding of an SN/VTA response to social cues after isolation supports the idea that positive social interactions are indeed a basic human need and that acute loneliness is an unpleasant state that motivates people to repair what is lacking, similar to hunger. The researchers indicated that a vital next question is how much and what kinds of positive social interaction are sufficient to fulfill social needs and thus eliminate the neural craving response.2
Budget Policy:
The FY 2023 President’s Budget request for extramural basic research (non-pain) is $28.7 million, a decrease of $0.8 million compared with the FY 2022 CR level.
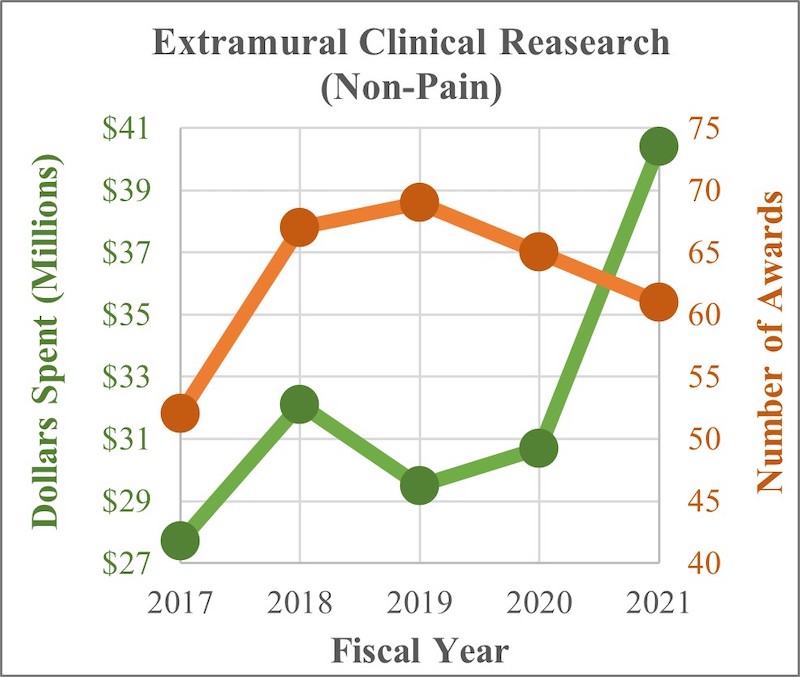
Extramural Clinical Research (Not Pain Related)

The NCCIH extramural clinical research program supports trials of complementary and integrative health approaches, including early- and mid-phase testing to assess biological signatures of these interventions in humans (and replication of these effects), define appropriate dosage, refine the components and mode of intervention delivery, determine optimal frequency or duration of the intervention, assess feasibility, and enhance adherence. The Center also supports later stage full-scale efficacy and effectiveness trials when the evidence base is sufficient to justify them. When interventions have been found effective, the Center supports pragmatic or implementation trials to integrate the interventions into health care systems. The following is an example of research supported by this program.
Researchers from New York University Grossman School of Medicine and Boston University compared the effect of Kundalini yoga to cognitive behavioral therapy (CBT) for the treatment of generalized anxiety disorder (GAD). GAD is a condition in which people feel extremely worried about things like health, money, or family problems, even when there’s little reason to worry about them. People with GAD find it hard to control their anxiety and focus on other things. CBT is an effective first-line, evidence-based psychotherapy for GAD, but many people do not receive CBT because of cost, stigma, or logistical reasons. Increasingly, people are seeking alternative interventions, such as yoga, outside the medical system. This study sought to help fill a knowledge gap on the potential benefits of yoga for GAD and how it compares to CBT. The study was a randomized, controlled, single-blind clinical trial with 230 participants. Each participant was assigned to one of three interventions: Kundalini yoga, CBT, and a control stress education course. The researchers found that Kundalini yoga was helpful for adults with GAD but not as effective as CBT. However, they noted that given the increasing costs of health care and barriers to accessing trained mental health professionals, yoga may play a role in GAD management as a more easily accessible intervention.3
Budget Policy:
The FY 2023 President’s Budget request for extramural clinical research (non-pain) is $40.6 million, an increase of $0.8 million compared with the FY 2022 CR level.
Extramural Pain and Pain Management Research

Pain is a major public health problem and is the most common reason why Americans use complementary and integrative health practices. Therefore, NCCIH has made pain management a major emphasis in its research efforts. The NCCIH extramural pain and pain management research program supports basic and clinical research on the biological basis of pain and the development, evaluation, and implementation of complementary and integrative pain management techniques. The following is an example of research supported by this program.
The NIH-DoD-VA Pain Management Collaboratory: The Impact of the Stepped-Care Model for Pain Management
In 2017, NCCIH partnered with the DoD, the VA, and seven other Institutes and Centers at the NIH to launch the NIH-DoD-VA Pain Management Collaboratory. The Collaboratory develops, supports, and enacts the implementation of large-scale, pragmatic clinical research in military and veteran health care delivery organizations to study nonpharmacologic approaches to pain management in innovative and integrative models of pain care delivery. The Stepped-Care Model for Pain Management (SCM-PM) is one area of investigation.
The SCM-PM is a tiered treatment plan that escalates from low-risk and broadly accessible interventions to higher risk and more specialized interventions based on a patient’s need. This approach to pain management has been implemented throughout the Veterans Health Administration (VHA) and Military Health System (MHS) since 2009.
Results from Collaboratory-supported studies are just beginning to be published. The following are the results from two supported investigative teams.
A study evaluated how the implementation of SCM-PM has impacted pain management culture within the VHA. They found that after 10 years the VHA pain management culture has shifted from a reliance on opioid treatments to a greater focus on nonpharmacologic approaches. The SCM-PM has encouraged multidisciplinary teams to work together to ensure that veterans receive coordinated pain care. Despite general acceptance, most VA facilities do not have a clear treatment “roadmap” for utilizing nonpharmacologic approaches.1 This is an area of implementation research the Collaboratory is working to address.
Another study evaluated the acceptance and impact of SCM-PM for the treatment of knee pain within the MHS. They found that the majority of care evaluated followed the SCM-PM guidelines, with 89.7 percent of patients only requiring step 1 (low-risk) level care. The patients who required additional care had lower long-term costs, fewer visits, and fewer recurrences of knee pain than patients who did not follow the SCM-PM guidelines.2 These findings demonstrate the value of SCM-PM and encourage its use.
1Mattocks, K. et al. Pain. Med. (2020).
2Garcia, A. et al. Am. J. Med. (2021).
Researchers from Stanford University found that a single 2-hour pain self-management skills class is no less effective than an 8-week, 16-hour cognitive behavioral therapy (CBT) program for reducing pain catastrophizing, pain intensity, and pain interference in adults with chronic low-back pain. Previous research had shown that a CBT program that focuses on pain self-management skills can help people with chronic low-back pain feel better, at least in part by reducing pain catastrophizing (a pattern of response that includes paying a lot of attention to the pain and feeling helpless). However, because CBT typically involves 8 to 12 group sessions, some people may not be able to participate because of time, cost, or limited availability of therapists. More rapid and efficient options would be valuable. The investigators who conducted this study wanted to know if a single 2-hour pain self-management skills class could be as effective as CBT. In the study, 263 adults with chronic low-back pain were randomly assigned to a single 2-hour pain relief skills class, an 8-session (16-hour) group CBT program, or a single 2-hour back pain health education class that did not teach pain management skills. The study indicated that a single pain management skills class can have meaningful benefits for patients with chronic low-back pain. The researchers suggested that this new intervention could improve access to care due to its adaptability and low cost. They cautioned, however, that the study’s participants were mostly White and of high socioeconomic status. More research is needed to determine if similar results can be obtained with participants of different socioeconomic status or in racially/ethnically diverse populations 4
Budget Policy:
The FY 2023 President’s Budget request for extramural pain and pain management research is $66.0 million, an increase of $26.0 million compared with the FY 2022 CR level.
The NCCIH Epidemiology Program
The NCCIH epidemiology program designs, implements, and analyzes high-quality surveys and longitudinal studies to further the understanding of complementary health approaches, chronic pain, health, and well-being. The team uses both quantitative and qualitative epidemiologic research methods to explore topics such as the prevalence, costs, and reasons for use of complementary health treatments and practices, and disparities in pain and its management. The following are some of the recent analyses conducted through this program.
An analysis of data from the National Ambulatory Medical Care Survey found an underuse of nonpharmacologic and an overuse of pharmacologic treatments for chronic musculoskeletal pain in youth, despite safety and effectiveness evidence for nonpharmacologic approaches and their inclusion in clinical guidelines. The researchers noted that finding ways to increase health care providers’ use of evidence-based nonpharmacologic options is an important next step for treating chronic pain in youth.1
An analysis of data from the National Health Interview Survey (NHIS) found differences in pain among U.S. subpopulations based on race and Hispanic ancestry. The data showed that many Hispanic subpopulations exhibited lower prevalence of pain than White non-Hispanics; however, pain prevalence for some Hispanic subpopulations was equivalent to or greater than that of White non-Hispanics. These data highlight important differences in reported pain among U.S. subpopulations. More research is needed to determine if these differences are biological, cultural, or procedural.2
Another analysis of data from the NHIS explored the relationship between pain and cognitive impairment (CI). Researchers found that pain and CI increase each other’s severity. Interactions between pain and CI were associated with poorer health status, higher health care use, and more disability than those seen in individuals with only pain or only CI. The researchers suggested that these results may encourage health care providers and family members caring for people with CI to regularly assess and manage them for pain.3
1Feldman, DE et al. J. Pediatr. (2021).
2Nahin, RL et al. J. Pain. (2021).
3Nahin, RL et al. Clin. J. Pain. (2020).
Intramural Research
The NCCIH Division of Intramural Research conducts basic, clinical, and translational research focusing on the role of the nervous system, other physiological systems, and psychosocial factors in perceiving, modifying, and managing pain, with the long-term goal of improving clinical management of chronic pain through the integration of pharmacologic and nonpharmacologic approaches. Research projects include investigating the role of the brain in pain processing and control, and how factors such as emotion, attention, environment, and genetics affect pain perception. The program includes research that explores how chronic pain produces changes in the brain that can modify how the brain reacts to pain medications such as opioids. The program both engages and leverages the exceptional basic and clinical research talent and resources of other neuroscience and neuroimaging efforts within the NIH intramural community. The NCCIH intramural program provides a rich environment for the training and development of clinical and basic scientists. The following is an example of research supported by this program.
NCCIH researchers compared the neural effects of placebo pain relief in people with fibromyalgia and healthy individuals. Fibromyalgia is a common disorder that involves widespread pain, tenderness, fatigue, and other symptoms. People with fibromyalgia and other individuals with chronic pain have anatomical, functional, and neurochemical changes in brain regions and neural pathways involved in placebo analgesia (pain relief in response to a “medicine” that contains no active pain-relieving ingredients). In a recent study, researchers investigated whether people with fibromyalgia differ from healthy control subjects in their behavioral and neural responses to placebo pain relief. In this study, 32 participants with mild-to-moderate fibromyalgia and chronic pain were matched with 46 healthy control subjects. These participants underwent placebo analgesic experiments during fMRI scans. The investigators found that there was no difference between the participants with fibromyalgia and the healthy control subjects in either pain intensity ratings or neural placebo-related responses, indicating that the placebo effect in individuals with fibromyalgia is comparable to that of healthy control subjects. Across all participants, placebo analgesia resulted in decreased pain intensity and unpleasantness ratings, less pain-related activity within the brain’s right insula and bilateral secondary somatosensory cortex, and reduced neurologic pain signature response. The results of this study also suggested that the placebo effects were driven more by conditioning than expectation. These findings might unveil new therapeutic strategies for people with chronic pain. The researchers recommend that future studies evaluate fibromyalgia patients who have more severe pain and disease burden to determine how these factors might affect placebo analgesia.5
Budget Policy:
The FY 2023 President’s Budget request for intramural research is $16.2 million, an increase of $1.5 million compared with the FY 2022 CR level.
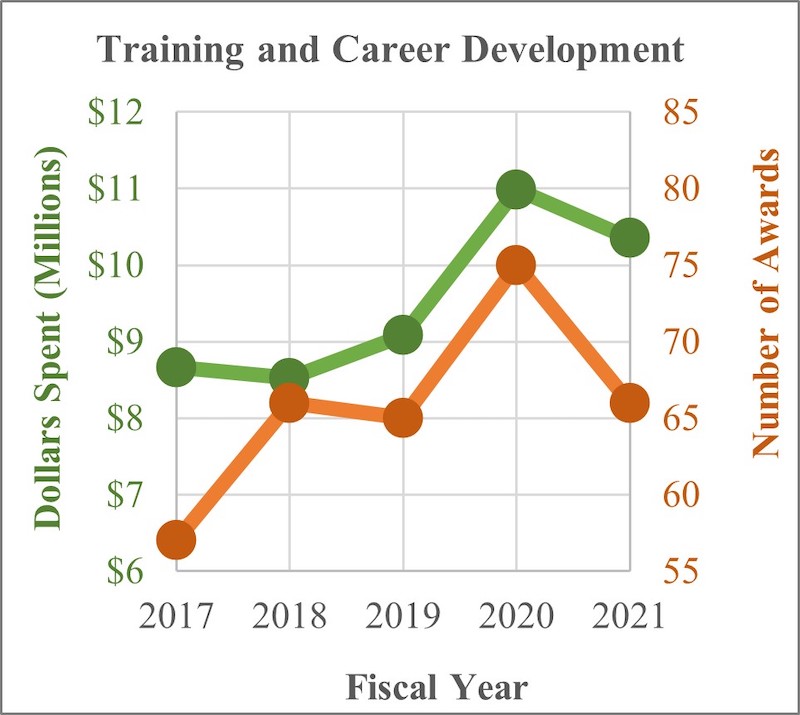
Extramural Research Training and Capacity Building

Improving the capacity of the field to carry out rigorous research on complementary and integrative health approaches is a priority for the NCCIH. To increase the number, quality, and diversity of investigators conducting this research, NCCIH supports a variety of training and career development activities for predoctoral students, postdoctoral fellows, and early-career investigators. NCCIH’s training strategies include innovative approaches that incorporate an understanding of the wide variety of modalities and specializations represented in the complementary and integrative health fields. In addition to scientists trained in key biomedical and behavioral research disciplines, the Center has opportunities for clinician-scientists, including conventionally trained physicians, complementary health practitioners, and other health care professionals (e.g., clinical psychologists, nurses) who conduct research across a wide range of complementary and integrative health approaches, including a program to support research training for clinicians through the National Clinical and Translational Science Awards (CTSA) Program. NCCIH also has career development funding opportunities for individuals from groups who are underrepresented in scientific research (e.g., racial and ethnic minority populations) and are interested in careers in complementary and integrative health research. In addition to these funding initiatives, NCCIH supports workshops to help students and fellows connect to NIH funding opportunities, understand how to interact with NIH staff to develop research proposals, navigate the NIH peer review process successfully, develop resilience to overcome career roadblocks, and develop plans for a successful research career. The following is an example of recently published results from a supported investigator.
A clinician-scientist supported through a career development award helped develop a new metric for measuring mental states during meditation. Meditation practices are often used to promote interoception, an internally oriented attention to bodily sensations. However, exactly how meditation impacts internal attention states, such as the focus on breath, has been unclear because of a lack of measurement tools to objectively assess mental states during meditation. This study aimed to address this measurement gap. The team of researchers from the University of Texas at Austin, University of Toronto, University of Wisconsin-Madison, and University of California, San Francisco tested the feasibility of applying multi-voxel pattern analysis (MVPA) to single-subject fMRI neural data to learn and recognize internal attention states important for breath-focused meditation. The results of this study have helped make invisible internal processes visible and quantifiable. The researchers concluded that their findings establish the feasibility of using MVPA classifiers to objectively assess mental states during meditation. The development of measures to precisely assess the attentional qualities cultivated by meditation may provide the measurement power needed to rigorously test the attentional and emotional mechanisms through which meditation may improve health and well-being6
Budget Policy:
The FY 2023 President’s Budget request for extramural research training and capacity is $10.1 million, a decrease of $0.5 million compared with the FY 2022 CR level.
Research Management Support (RMS)

Through its RMS activities, NCCIH provides administrative, budgetary, information technology, logistical, and scientific support in the review, award, monitoring, and management of research grants, training awards, and contracts. RMS functions also encompass strategic planning, coordination, and evaluation of programs. The Center uses Qlik Sense, a data analytics platform, to compile interactive reports and enhanced dashboards to provide NCCIH leadership with trend data and performance indicators to ensure responsible stewardship of public funds. In addition to these activities, NCCIH disseminates objective, evidence-based information to the public, scientists, and health care providers to help them make informed decisions about the use of complementary and integrative health practices. All information is freely available on the NCCIH website (nccih.nih.gov) or through the NCCIH Information Clearinghouse.
Budget Policy:
The FY 2023 President’s Budget request for RMS is $21.8 million, an increase of $2.2 million compared with the FY 2022 CR level.
1Nahin RL, Barnes PM, Stussman BJ. Expenditures on complementary health approaches: United States, 2012. National Health Statistics Reports; no. 95. Hyattsville, MD: National Center for Health Statistics. 2016.
2Tomova L, Wang KL, Thompson T, et al. Acute social isolation evokes midbrain craving responses similar to hunger. Nature Neuroscience. 2020;23(12):1597-1605.
3Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20.
4Darnall BD, Roy A, Chen AL, et al. Comparison of a single-session pain management skills intervention with a single-session health education intervention and 8 sessions of cognitive behavioral therapy in adults with chronic low back pain: a randomized clinical trial. JAMA Network Open. 2021;4(8):e2113401.
5Frangos E, Čeko M, Wang B, et al. Neural effects of placebo analgesia in fibromyalgia patients and healthy individuals. Pain. 2021;162(2):641-652.
6Weng HY, Lewis-Peacock JA, Hecht FM, et al. Focus on the breath: brain decoding reveals internal states of attention during meditation. Frontiers in Human Neuroscience. 2020;14:336.
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Budget Authority by Object Class1
(Dollars in Thousands)
| FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 | |
|---|---|---|---|
| Total compensable work years: | |||
| Full-time equivalent | 90 | 100 | 10 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $0 | $0 | $0 |
| Average GM/GS grade | 13.3 | 13.4 | 0.1 |
| Average GM/GS salary | $119 | $120 | $2 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $146 | $152 | $7 |
| Average salary of ungraded positions | $186 | $195 | $9 |
| OBJECT CLASSES | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 |
|---|---|---|---|
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | 7,800 | 8,978 | 1,178 |
| 11.3 Other Than Full-Time Permanent | 2,703 | 3,113 | 410 |
| 11.5 Other Personnel Compensation | 416 | 480 | 65 |
| 11.7 Military Personnel | 107 | 122 | 15 |
| 11.8 Special Personnel Services Payments | 1,033 | 1,178 | 146 |
| 11.9 Subtotal Personnel Compensation | $12,058 | $13,871 | $1,813 |
| 12.1 Civilian Personnel Benefits | 5,144 | 5,761 | 617 |
| 12.2 Military Personnel Benefits | 63 | 72 | 9 |
| 13.0 Benefits to Former Personnel | 0 | 0 | 0 |
| Subtotal Pay Costs | $17,265 | $19,704 | $2,439 |
| 21.0 Travel & Transportation of Persons | 257 | 291 | 34 |
| 22.0 Transportation of Things | 15 | 17 | 2 |
| 23.1 Rental Payments to GSA | 0 | 0 | 0 |
| 23.2 Rental Payments to Others | 0 | 0 | 0 |
| 23.3 Communications, Utilities & Misc. Charges | 41 | 47 | 6 |
| 24.0 Printing & Reproduction | 0 | 0 | 0 |
| 25.1 Consulting Services | 5,940 | 6,349 | 409 |
| 25.2 Other Services | 4,991 | 5,549 | 558 |
| 25.3 Purchase of goods and services from Government Accounts | 14,588 | 14,803 | 215 |
| 25.4 Operation & Maintenance of Facilities | 3 | 4 | 0 |
| 25.5 R&D Contracts | 1,410 | 1,487 | 78 |
| 25.6 Medical Care | 38 | 40 | 2 |
| 25.7 Operation & Maintenance of Equipment | 251 | 272 | 21 |
| 25.8 Subsistence & Support of Persons | 0 | 0 | 0 |
| 25.0 Subtotal Other Contractual Services | $27,221 | $28,504 | $1,283 |
| 26.0 Supplies & Materials | 328 | 369 | 41 |
| 31.0 Equipment | 376 | 424 | 48 |
| 32.0 Land and Structures | 0 | 0 | 0 |
| 33.0 Investments & Loans | 0 | 0 | 0 |
| 41.0 Grants, Subsidies & Contributions | 108,658 | 134,012 | 25,353 |
| 42.0 Insurance Claims & Indemnities | 0 | 0 | 0 |
| 43.0 Interest & Dividends | 0 | 0 | 0 |
| 44.0 Refunds | 0 | 0 | 0 |
| Subtotal Non-Pay Costs | $136,897 | $163,664 | $26,767 |
| Total Budget Authority by Object Class | $154,162 | $183,368 | $29,206 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 |
|---|---|---|---|
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $7,800 | $8,978 | $1,178 |
| Other Than Full-Time Permanent (11.3) | 2,703 | 3,113 | 410 |
| Other Personnel Compensation (11.5) | 416 | 480 | 65 |
| Military Personnel (11.7) | 107 | 122 | 15 |
| Special Personnel Services Payments (11.8) | 1,033 | 1,178 | 146 |
| Subtotal Personnel Compensation (11.9) | $12,058 | $13,871 | $1,813 |
| Civilian Personnel Benefits (12.1) | $5,144 | $5,761 | $617 |
| Military Personnel Benefits (12.2) | 63 | 72 | 9 |
| Benefits to Former Personnel (13.0) | 0 | 0 | 0 |
| Subtotal Pay Costs | $17,265 | $19,704 | $2,439 |
| Travel & Transportation of Persons (21.0) | $257 | $291 | $34 |
| Transportation of Things (22.0) | 15 | 17 | 2 |
| Rental Payments to Others (23.2) | 0 | 0 | 0 |
| Communications, Utilities & Misc. Charges (23.3) | 41 | 47 | 6 |
| Printing & Reproduction (24.0) | 0 | 0 | 0 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | 5,940 | 6,349 | 409 |
| Other Services (25.2) | 4,991 | 5,549 | 558 |
| Purchases from Government Accounts (25.3) | 14,588 | 14,803 | 215 |
| Operation & Maintenance of Facilities (25.4) | 3 | 4 | 0 |
| Operation & Maintenance of Equipment (25.7) | 251 | 272 | 21 |
| Subsistence & Support of Persons (25.8) | 0 | 0 | 0 |
| Subtotal Other Contractual Services | $25,773 | $26,977 | $1,204 |
| Supplies & Materials (26.0) | $328 | $369 | $41 |
| Subtotal Non-Pay Costs | $26,415 | $27,701 | $1,287 |
| Total Administrative Costs | $43,680 | $47,406 | $3,726 |
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Full-Time Equivalent Employment (FTE)
| OFFICE/DIVISION | FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of Extramural Activities | |||||||||
| Direct: | 5 | - | 5 | 7 | - | 7 | 7 | - | 7 |
| Total: | 5 | - | 5 | 7 | - | 7 | 7 | - | 7 |
| Office of the Director | |||||||||
| Direct: | 6 | - | 6 | 5 | - | 5 | 6 | - | 6 |
| Total: | 6 | - | 6 | 5 | - | 5 | 6 | - | 6 |
| Office of Administrative Operations | |||||||||
| Direct: | 17 | - | 17 | 20 | - | 20 | 21 | - | 21 |
| Total: | 17 | - | 17 | 20 | - | 20 | 21 | - | 21 |
| Office of Policy, Planning, and Evaluation | |||||||||
| Direct: | 4 | - | 4 | 3 | - | 3 | 4 | - | 4 |
| Total: | 4 | - | 4 | 3 | - | 3 | 4 | - | 4 |
| Office of Communications and Public Liaison | |||||||||
| Direct: | 8 | - | 8 | 10 | - | 10 | 12 | - | 12 |
| Total: | 8 | - | 8 | 10 | - | 10 | 12 | - | 12 |
| Office of Clinical and Regulatory Affairs | |||||||||
| Direct: | 4 | - | 4 | 5 | - | 5 | 6 | - | 6 |
| Total: | 4 | - | 4 | 5 | - | 5 | 6 | - | 6 |
| Division of Extramural Research | |||||||||
| Direct: | 14 | - | 14 | 18 | - | 18 | 20 | - | 20 |
| Reimbursable: | 2 | - | 2 | 2 | - | 2 | 2 | - | 2 |
| Total: | 16 | - | 16 | 20 | - | 20 | 22 | - | 22 |
| Division of Intramural Research Program | |||||||||
| Direct: | 10 | 1 | 11 | 13 | 1 | 14 | 14 | 1 | 15 |
| Total: | 10 | 1 | 11 | 13 | 1 | 14 | 14 | 1 | 15 |
| Office of scientific Review | |||||||||
| Direct: | 4 | - | 4 | 2 | - | 2 | 3 | - | 3 |
| Total: | 4 | - | 4 | 2 | - | 2 | 3 | - | 3 |
| Office of Grants Management | |||||||||
| Direct: | 3 | - | 3 | 4 | - | 4 | 4 | - | 4 |
| Total: | 3 | - | 3 | 4 | - | 4 | 4 | - | 4 |
| Total | 77 | 1 | 78 | 89 | 1 | 90 | 99 | 1 | 100 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTEs supported by funds from Cooperative Research and Development Agreements. | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| FISCAL YEAR | Average GS Grade | ||||||||
| 2019 | 13.2 | ||||||||
| 2020 | 13.3 | ||||||||
| 2021 | 13.2 | ||||||||
| 2022 | 13.3 | ||||||||
| 2023 | 13.4 | ||||||||
NATIONAL INSTITUTES OF HEALTH
National Center for Complementary and Integrative Health
Detail of Positions1
| GRADE | FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget |
|---|---|---|---|
| Total, ES Positions | 0 | 0 | 0 |
| Total, ES Salary General Schedule | $0 | $0 | $0 |
| GM/GS-15 | 13 | 13 | 13 |
| GM/GS-14 | 15 | 15 | 15 |
| GM/GS-13 | 22 | 28 | 34 |
| GS-12 | 14 | 17 | 20 |
| GS-11 | 3 | 3 | 0 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 1 | 3 | 5 |
| GS-8 | 0 | 0 | 0 |
| GS-7 | 1 | 2 | 3 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 0 | 0 | 0 |
| GS-3 | 0 | 0 | 0 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 69 | 81 | 90 |
| Commissioned Corps (42 U.S.C. 207) | |||
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 1 | 1 | 1 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 1 | 1 | 1 |
| Ungraded | 28 | 28 | 29 |
| Total permanent positions | 67 | 79 | 89 |
| Total positions, end of year | 98 | 110 | 120 |
| Total full-time equivalent (FTE) employment, end of year | 78 | 90 | 100 |
| Average ES salary | $0 | $0 | $0 |
| Average GM/GS grade | 13.2 | 13.3 | 13.4 |
| Average GM/GS salary | $128,152 | $118,546 | $120,485 |
| 1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||